3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(12):2653-2660. doi:10.7150/ijms.49857 This issue Cite
Research Paper
Predictability of Macrosomic Birth based on Maternal Factors and Fetal Aneuploidy Screening Biochemical Markers in Hyperglycemic Mothers
1. Department of Biomedical Sciences, University of North Dakota, Grand Forks, North Dakota, USA.
2. YooJin BioSoft Co., Ltd., Goyang, Gyeonggi-do 10403, Korea.
3. Department of Food and Nutrition, Inha University, Incheon 22212, Korea.
4. Department of Biomedical Science, CHA University, Seongnam-Si, Gyeonggi-Do 13488, Korea.
5. Department of Obstetrics and Gynecology, College of Medicine, Ewha Womans University, 1071 Anyangcheon-ro, Yangcheon-gu, Seoul 07985, Korea.
6. Department of Obstetrics and Gynecology, Korea University Medicine, Seoul 02841, Korea.
7. Department of Public Health, Korea University Graduate School, Seoul 02841, Korea.
Abstract
Background: Macrosomic birth weight has been implicated as a significant risk factor for developing various adult metabolic diseases such as diabetes mellitus and coronary heart diseases; it has also been associated with higher incidences of complicated births. This study aimed to examine the predictability of macrosomic births in hyperglycemic pregnant women using maternal clinical characteristics and serum biomarkers of aneuploidy screening performed in the first half of pregnancy.
Methods: A retrospective observational study was performed on a cohort of 1,668 pregnant women who 1) had positive outcomes after undergoing 50-g oral glucose challenge test (OGCT) at two university-based hospitals and 2) underwent any one of the following maternal biomarker screening tests for fetal aneuploidy: triple test, quadruple test, and integrated test. Logistic regression-based models for predicting macrosomic births using maternal characteristics and serum biomarkers were developed and evaluated for prediction power. A nomogram, which is a graphical display of the best predictable model, was then generated.
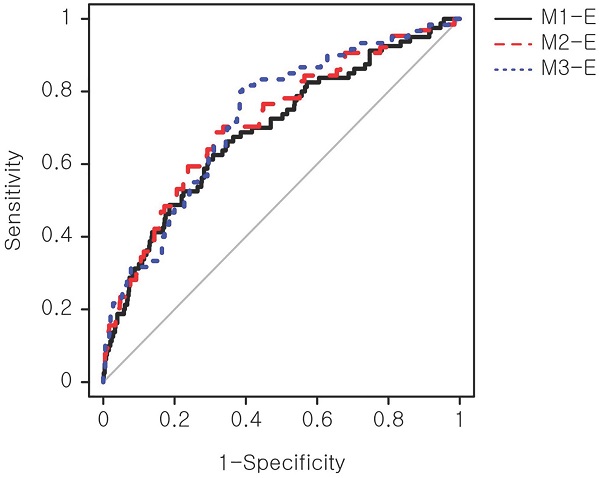
Results: The study cohort included 157 macrosomic birth cases defined as birth weight ≥3,820 g, which was equivalent to the top 10 percentile of the modeling cohort. Three primary models solely based on serum biomarkers achieved area under curves (AUCs) of 0.55-0.62. Expanded models, including maternal demographic and clinical factors, demonstrated an improved performance by 25% (AUCs, 0.69-0.73).
Conclusion: Our prediction models will help to identify pregnancies with an elevated risk of macrosomic births in hyperglycemic mothers using maternal clinical factors and serum markers from routine antenatal screening tests. Prediction of macrosomic birth at mid-pregnancy may allow customized antenatal care to reduce the risk of macrosomic births.
Keywords: maternal biomarker, macrosomic births, maternal hyperglycemia, nomogram

 Global reach, higher impact
Global reach, higher impact