Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(14):3565-3580. doi:10.7150/ijms.115853 This issue Cite
Research Paper
Causal Effects of Exposure to Air Pollution on the Risk of Neurosurgical Multi-system Diseases: A Worldwide Study of Mendelian Randomization
Department of Neurosurgery, West China Hospital of Sichuan University, Sichuan University, Chengdu, Sichuan, China.
Received 2025-4-16; Accepted 2025-7-16; Published 2025-7-28
Abstract
Background: Epidemiological studies has investigated the correlation between ambient air pollution and neurosurgical multisystem diseases. Multiple studies have shown that air pollution significantly influences various neurological disorders. Nevertheless, the findings from these studies are inconsistent and contentious, leaving the causal relationships for many conditions unresolved. The study systematically investigates the underlying genetic causal relationships between air pollution and neurosurgical multisystem diseases, as well as to assess the implications of these associations.
Methods: Genetic instruments for particulate matter (PM) with aerodynamic diameter < 2.5 μm (PM2.5), < 2.5-10 μm (PM2.5-10), <10 μm (PM10), PM2.5 absorbance, nitrogen dioxide (NO2), nitrogen oxides (NOx) and 30 neurosurgical multi-system diseases were selected.
Results: In the European population, a noteworthy causal association was identified between NO2 and PM2.5 exposure and cerebral infarction (IVW: OR = 1.03, 95%CI: 1.01~1.06). Among African American or Afro-Caribbean individuals, NOx (IVW: OR = 0.63, 95%CI: 0.44~0.90) and NO2 (IVW: OR = 0.68, 95%CI: 0.54-0.87) are predisposed to trigger trigeminal neuralgia, while PM2.5 is related to 3 neurosurgical diseases, including epilepsy (IVW: OR = 0.89, 95%CI: 0.79~1.00), subarachnoid hemorrhage (IVW: OR = 0.75, 95%CI: 0.61~0.91), and diffuse brain injury (IVW: OR = 0.67, 95%CI: 0.47~0.96). In East Asian populations, a correlation has been observed between PM2.5 (IVW: OR = 0.99, 95%CI: 0.98~1.00) and PM10 (IVW: OR = 1.00, 95%CI: 1.00~1.00) exposure and the occurrence of cervical spondylosis. Additionally, there is a genetic susceptibility to pituitary adenoma and craniopharyngioma related to NO2 (IVW: OR = 1.24, 95%CI: 1.02~1.52) and PM2.5 absorbance (IVW: OR = 0.73, 95%CI: 0.59~0.90). In South Asian populations, there is a significant genetic susceptibility to the influences of PM2.5-10 (IVW: OR = 0.90, 95%CI: 0.83~0.97) on stroke incidence. In contrast, for populations in the Greater Middle East, air pollution is predominantly associated with cerebrovascular diseases. For example, PM2.5-10 shows a positive genetic predisposition towards stroke (IVW: OR = 1.02, 95%CI: 1.00~1.05) and subarachnoid hemorrhage (IVW: OR = 1.06, 95%CI: 1.00~1.12).
Conclusion: This study presents the first genetic evidence establishing a connection between air pollution and neurosurgical multisystem diseases. Our findings emphasize the importance of air quality in the context of these diseases, potentially offering new insights into the underlying mechanisms and informing future clinical research on air pollution-mediated neurosurgical conditions, particularly cerebrovascular and brain functional disorders.
Keywords: air pollution, neurosurgical multi-system diseases, Mendelian randomization, genetic associations
1. Introduction
Emerging evidence suggests that ambient air pollution, comprising complex mixtures of various PM and NOx [1], poses multiple adverse hazards to human health and may elevate the morbidity and mortality rates of cardiovascular, cerebrovascular, and oncological diseases [2, 3]. Studies have showed that air pollution can enhance the risk of mortality from non-communicable diseases by nearly 20% [2]. Notably, air pollution and the occurrence of neurosurgical multisystem diseases has underlying correlation. The neurosurgical multisystem diseases here are classified into five major categories based on clinical experience, including functional diseases, cerebrovascular diseases, Spinal and spinal cord diseases, central nervous system neoplasms and Other brain diseases, which facilitates our summary of the relationship between different types of neurosurgical diseases and environmental pollution (Details in Figure 1). Since the 1990s, epidemiological data from multiple research teams across North America, Asia, and Europe have demonstrated a correlation between air pollution and cerebrovascular disease mortality. Regions with elevated gaseous pollutants, including PM2.5 and ozone, have experienced a significant increase in cerebrovascular accidents [4]. Furthermore, numerous studies have also explored the influence of air pollution on other neurological disorders. For example, Shreya Louis et al. found that epilepsy is closely associated with air pollution and temperature, while long-term and short-term exposure to air pollution, such as PM2.5, PM10, PM2.5-10 and NOx were significantly associated with ischemic stroke and transient ischemic attack [3]. Ma et al. discovered that prolonged exposure to high concentrations of PM2.5 can lead to the accumulation of amyloid protein, thereby heightening the risk of cognitive impairment and influencing the neurobiological characteristics associated with Alzheimer's disease [5]. Additionally, study has indicated that exposure to air pollution is relevant to increase of risk both benign [6] and malignant brain tumors [7]. However, further investigation is required to elucidate the specific types of tumors involved and the underlying mechanisms of their development.
Therefore, the influence of ambient air pollution on neurosurgical multi-system diseases cannot be ignored [8-10], and these pollutants bring a heavy burden to the human body and aggravate the comorbidities [11]. Nowadays, many prospective studies and epidemiological investigations have displayed that air pollution is highly relevant to a variety of neurological diseases, such as stroke [12], Alzheimer's disease [13], Parkinson's disease [14] and epilepsy [15]. Due to the regional or population-specific focus of these studies, rather than utilizing a diverse array of clinical samples across various races and regions, the findings are subject to confounding factors and lack systematic generalizability. The aim of this study is to systematically survey the correlation between neurosurgical multi-system diseases and air pollution across different races and populations using Mendelian randomization analysis. Furthermore, it seeks to comprehensively summarize the impact of air pollution on neurological diseases, and provide research basis for guiding neurosurgeons to treat related diseases and local governments to control air pollution.
Our study indicates that genetic polymorphisms can enhance our comprehension of environmental health risks. To address the aforementioned methodological challenges, we utilized Mendelian randomization (MR) analysis [16]. The MR approach, grounded in Mendel's second law of inheritance to mitigate confounding factors [17], utilizes genetic variation as instrumental variables (IVs) to evaluate the correlation between air pollution and neurosurgical multisystem diseases. We proceeded the two-sample MR analysis applying data from genome-wide association studies (GWAS) [18]and UK Biobank [19] data in this research. It is noteworthy that, in recent years, numerous researchers have employed MR techniques to probe underlying relationships between ambient air pollution and various tumors [7], adverse pregnancy [20], cardiovascular disease [21], autoimmune disease [22], chronic obstructive pulmonary disease [23], cognitive ability [24], and amyotrophic lateral sclerosis [25]. However, to date, no researchers have applied MR methods to study the effects of air pollution on neurological diseases.
Therefore, this study aims to utilize comprehensive data on ambient air pollution and neurosurgical multisystem diseases to elucidate their causal relationship, thereby informing strategies to mitigate the influence of air pollution on neurological conditions through public health prevention and intervention measures.
2. Methods
2.1. Overall research design
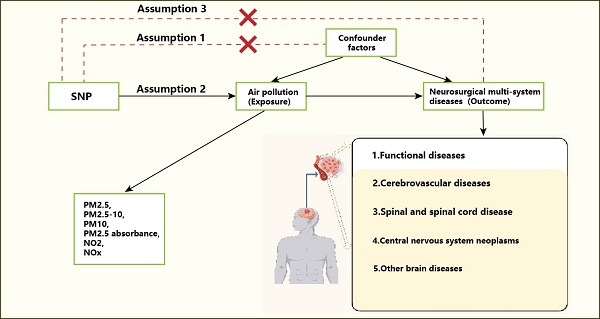
Figure 1 elucidates the whole study design. We adopted MR analysis to survey the causal correlation between ambient air pollution and neurosurgical multisystem diseases. The study followed strictly to the STROBE-MR guidelines [26] and was meticulously designed based on three key hypotheses, including: 1. The IVs in this study are genetic variations closely related to ambient air pollution, specifically SNPs. 2. These genetic variations are not relevant to confounding variables and influence disease outcomes solely through the specific exposure under investigation. 3. The genetic variants impact neurological diseases exclusively via ambient air pollution, without involvement of alternative pathways [27]. Previous studies have confirmed that particulate matter and nitrogen oxides can directly damage the central nervous system by disrupting the blood-brain barrier, causing neuroinflammation and oxidative stress [28]. Therefore, this study mainly selected PM2.5, PM2.5-10, PM10, PM2.5 absorbance, NO2 and NOx for in-depth research. For O₃ and SO₂, due to significant data gaps in O₃ monitoring and a notable decrease in SO₂ concentration in recent years, which limited the epidemiological association analysis, they were not included in this study. The diseases discussed in this study include 30 neurological diseases.
2.2. Summary datasets and populations
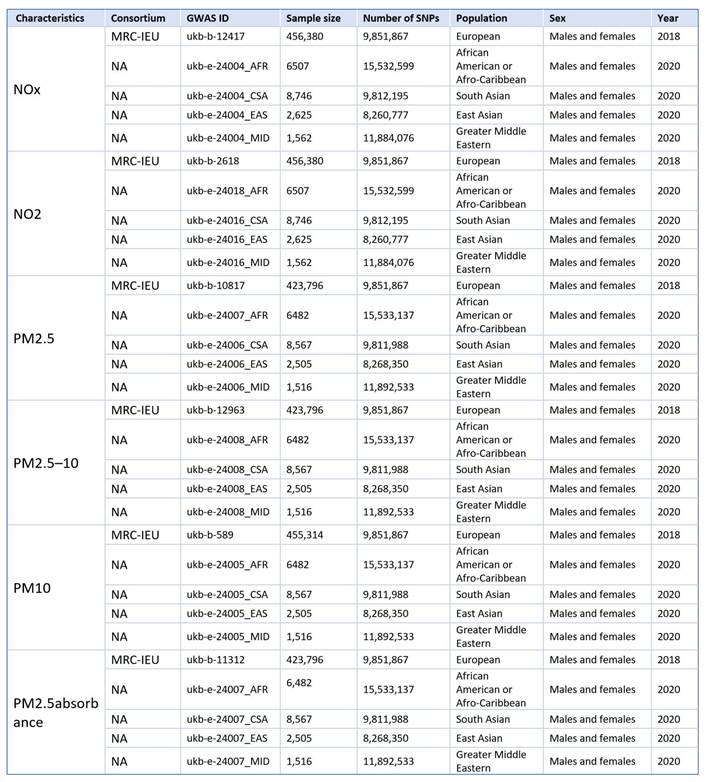
We obtained ambient air pollution via IEU Open GWAS (https://gwas.mrcieu.ac.uk/) [29] database as exposure factors for populations of European, African American or Afro-Caribbean, South Asian, East Asian, and Greater Middle Eastern. Ambient air pollution is caused by various air pollution, such as PM2.5, PM10, PM2.5-10, NOx, suspended particles (TSP), carbon oxides (CO, CO2), hydrocarbons (CH4) and other harmful substances [30]. Since the 1990s, PM2.5 is the most widely studied air pollution, followed by nitrogen oxides such as NO2 and NOx [31]. In recent years, particles with an aerodynamic diameter of 2.5 to 10μm are also receiving increasing attention, and different pollution have different degrees of damage to human health [32]. Based on this, we selected the above pollutants as the main exposure factors for MR analysis (Fig.2).
The flow chart of the MR analysis and study design. A. MR assumption. 1. SNPs are not associated with confounder; 2. SNPs are strongly associated with air pollution; 3. SNPs influence neurosurgical multi-system diseases solely through air pollution. B. Analysis flow chart.
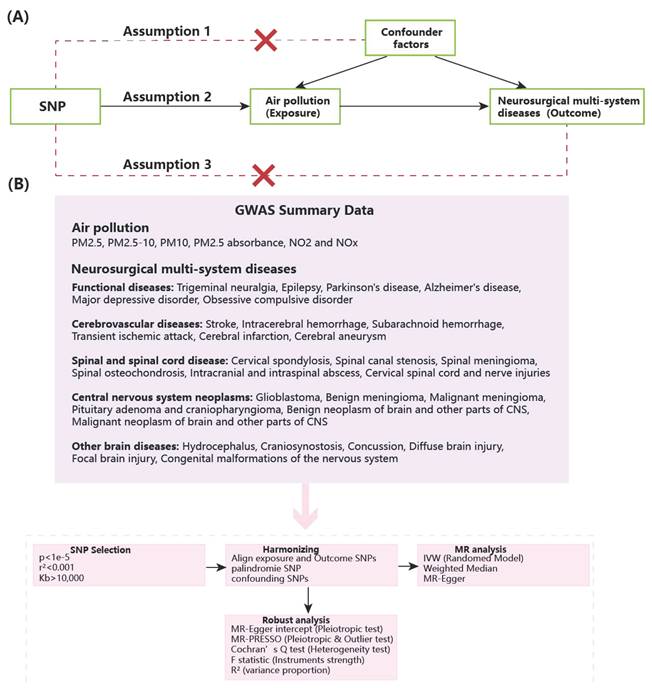
The GWAS database from Neale's lab provides the source of data on neurosurgical multisystem disorders, including Trigeminal neuralgia (195,847 cases), Epilepsy (458,310 cases), Parkinson's disease (480,018 cases), Alzheimer's disease (487,511 cases), Major depressive disorder (56,637 cases), Obsessive compulsive disorder (33,925 cases), Stroke (446,696 cases), Intracerebral hemorrhage (473,513 cases), Subarachnoid hemorrhage (473,255 cases), Transient ischemic attack (214,634 cases), Cerebral infarction (361,194 cases), Cerebral aneurysm (473,683 cases), Cervical spondylosis (484,598 cases), Spinal canal stenosis (454,787), Spinal meningioma (218,792 cases), Spinal osteochondrosis (164,865 cases), Intracranial and intraspinal abscess (217,626 cases), Cervical spinal cord and nerve injuries (215,730 cases), Glioblastoma (218,792 cases), Benign meningioma (218,792 cases), Malignant meningioma (218,792 cases), Pituitary adenoma and craniopharyngioma (218,792 cases), Benign neoplasm of brain and other parts of CNS (218,792 cases), Malignant neoplasm of brain and other parts of CNS (218,792 cases), Hydrocephalus (206,548 cases), Craniosynostosis (218,792 cases), Concussion (147,103), Diffuse brain injury (137,232 cases), Focal brain injury (137,641 cases) and Congenital malformations of the nervous system (218,792 cases) (Table 1). The above diseases in each major category are all common in clinical practice and also the most frequently encountered diseases in our daily operations in neurosurgery or in collaboration with the neurology department.
2.3. Selection of SNPs
To ascertain that ambient air pollution possesses a sufficient number of IVs to maintain statistical efficacy and meet the three hypothesis of MR analysis, we chose SNPs that demonstrated a strong relevance to air pollution (p<1e-5) (Table S1-S28). We employed thresholds of R²<0.001 and a distance greater than 10,000Kb to evaluate, identify, and exclude linkage disequilibrium (LD) effects, thereby ensuring the independence of the IVs. To mitigate the potential for horizontal pleiotropy and eliminate confounding variables, we utilized the PhenoScanner V2 database [33]. In addition, our choice of IVs also excluded palindromic SNPs to guarantee that the influences on exposure and outcomes correspond to the same alleles. To satisfy another assumption of MR analysis, we utilized the coefficient of determination (R²) as a genetic instrument to quantify the proportion of variance explained for traits, calculated as R² =2MAF×(1-MAF) (β / SD)². The F statistic was employed to assess the existence of weak IV bias and to determine the stability of individual SNPs. When F>10, SNPs are deemed to be undisturbed by weak IV bias, manifesting that the selected SNPs can precisely forecast exposure. The formula is as follows: F= [(K+1-N) R2] / [K(R2-1)]) [34]. K: variants, N: sample size (Fig.1).
2.4. Statistical analysis
In this study, inverse variance weighting (IVW) was primarily applied to estimate the relevance between air pollution and neurosurgical multi-system diseases, with weighted median (WM) and MR-Egger methods employed to further assess this correlation [35]. Sensitivity analyses incorporated heterogeneity analysis, horizontal pleiotropy analysis, and leave-one-out analysis. Cochran's Q statistic was applied to evaluate the heterogeneity of each MR association. P<0.05 for Cochran's Q statistic indicates heterogeneity exists, necessitating the use of a random effects model as the major method for subsequent testing [36]. MR-PRESSO method was assessed using MR-PRESSO outlier tests, corrected level pleiotropy (outlier test), and remarkable discrepancy in causal estimates before and after outlier adjustments [35]. Subsequently, a leave-one-out analysis was conducted to assess whether individual SNPs yielded remarkable consequences, thereby systematically excluding confounding SNPs [37]. Statistical analyses were proceeded applying R version 4.2.0 and the TwoSampleMR package version 0.6.3. A strong correlation was established when the results remained significant after applying the Bonferroni correction [38]. Furthermore, a strong correlation was deemed present if more than two distinct MR analyses yielded P-values less than 0.05. Even in cases where only a single method, particularly the IVW analysis, produced a P<0.05, the correlation was still deemed remarkable.
3. Results
3.1. MR analysis
To survey the relationship between ambient air pollution and neurosurgical multisystem diseases, we carried out the first global-scale MR analysis. Based on the variations in ambient air pollution, we proceeded with the subsequent analyses.
3.2. Causal effects of NOx on neurosurgical multisystem diseases
In the initial IVW, WM, and MR-Egger analyses, we utilized closely related SNPs as genetic instruments for investigating neurosurgical multisystem diseases (Fig.3 and Fig.4). Our consequences revealed a positive relativity between NOx and the dangerousness of spinal meningioma, and a negative relevance with the risk of major depressive disorder in the European population. NOx is negatively associated with the dangerousness of trigeminal neuralgia and cerebral aneurysm in African American or Afro-Caribbean population. NOx is positively correlation with the risk of focal brain injury in South Asian. And NOx is positively correlation with the risk of malignant neoplasm of brain and other parts of CNS in East Asian. However, no causal correlation has been discovered between NOx and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S1-S5).
Details of GWAS in the present study (outcome).
| Characteristics | Consortium | GWAS ID | Sample size | Number of SNPs | Population | Sex | Year | |
|---|---|---|---|---|---|---|---|---|
| Neurosurgical disorders | Diseases | |||||||
| functional diseases | Trigeminal neuralgia | NA | finn-b-G6_TRINEU | 195,847 | 16,380,408 | European | Males and females | 2021 |
| Epilepsy | NA | ebi-a-GCST90018840 | 458,310 | 24,186,492 | European | NA | 2021 | |
| Parkinson's disease | NA | ebi-a-GCST90018894 | 480,018 | 24,194,622 | European | NA | 2021 | |
| Alzheimer's disease | NA | ebi-a-GCST90027158 | 487,511 | 20,921,626 | European | NA | 2022 | |
| Major depressive disorder | NA | ebi-a-GCST90086059 | 56,637 | 11,498,420 | European | NA | 2021 | |
| Obsessive Compulsive Disorder | PGC | ieu-a-1189 | 33,925 | 8,409,517 | European | Males and females | 2017 | |
| cerebrovascular diseases | Stroke | NA | ebi-a-GCST005838 | 446,696 | 7,633,440 | European | NA | 2018 |
| Intracerebral hemorrhage | NA | ebi-a-GCST90018870 | 473,513 | 24,191,284 | European | NA | 2021 | |
| Subarachnoid hemorrhage | NA | ebi-a-GCST90018923 | 473,255 | 24,191,735 | European | NA | 2021 | |
| Transient ischemic attack | NA | finn-b-G6_TIA | 214,634 | 16,380,437 | European | Males and females | 2021 | |
| Cerebral infarction | NA | ukb-d-I63 | 361,194 | 10,889,323 | European | Males and females | 2018 | |
| Cerebral aneurysm | NA | ebi-a-GCST90018815 | 473,683 | 24,191,145 | European | NA | 2021 | |
| Spinal and spinal cord diseases | Cervical spondylosis | NA | ebi-a-GCST90038693 | 484,598 | 9,587,836 | European | NA | 2021 |
| Spinal canal stenosis | NA | ebi-a-GCST90018922 | 454,787 | 24,182,979 | European | NA | 2021 | |
| Spinal meningioma | NA | finn-b-CD2_BENIGN_MENINGES_SPINAL | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Spinal osteochondrosis | NA | finn-b-M13_SPINALOSTEOCHON | 164,865 | 16,380,216 | European | Males and females | 2021 | |
| Intracranial and intraspinal abscess | NA | finn-b-G6_CNSABSC | 217,626 | 16,380,461 | European | Males and females | 2021 | |
| Cervical spinal cord and nerve injuries | NA | finn-b-ST19_INJURY_NERVES_SPINAL_CORD_NECK_LEVEL | 215,730 | 16,380,463 | European | Males and females | 2021 | |
| central nervous system neoplasms | Glioblastoma | NA | finn-b-C3_GBM | 218,792 | 16,380,466 | European | Males and females | 2021 |
| Benign meningioma | NA | finn-b-CD2_BENIGN_MENINGES_CEREBRAL | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Malignant meningioma | NA | finn-b-C3_MENINGES | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Pituitary adenoma and craniopharyngioma | NA | finn-b-CD2_BENIGN_PITUITARY_CRANIPHAR | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Benign neoplasm of brain and other parts of CNS | NA | finn-b-CD2_BENIGN_BRAIN_CNS | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Malignant neoplasm of brain and other parts of CNS | NA | finn-b-C3_SPINAL_CORD_CRANIAL_AND_OTHER_CNS | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Other brain diseases | Hydrocephalus | NA | finn-b-G6_HYDROCEPH | 206,548 | 16,380,404 | European | Males and females | 2021 |
| Craniosynostosis | NA | finn-b-Q17_CRANIOSYNOSTOSIS | 218,792 | 16,380,466 | European | Males and females | 2021 | |
| Concussion | NA | finn-b-ST19_CONCUSSION | 147,103 | 16,380,074 | European | Males and females | 2021 | |
| Diffuse brain injury | NA | finn-b-ST19_DIFFU_BRAIN_INJURY | 137,232 | 16,379,965 | European | Males and females | 2021 | |
| Focal brain injury | NA | finn-b-ST19_FOCAL_BRAIN_INJURY | 137,641 | 16,379,970 | European | Males and females | 2021 | |
| Congenital malformations of the nervous system | NA | finn-b-Q17_CONGEN_MALFO_NERVOUS_SYSTEM | 218,792 | 16,380,466 | European | Males and females | 2021 | |
Details of GWAS in the present study (exposure).
3.3. Causal effects of NO2 on neurosurgical multisystem diseases
As for NO2, we found that NO2 was positively associated with cerebral infarction and craniosynostosis, and negatively correlation with concussion in the European population, where the association between NO2 and cerebral infarction and concussion was more robust. NO2 was negatively associated with trigeminal neuralgia and transient ischemic attack in African American or Afro-Caribbean population. NO2 was positively correlation with stroke, and negatively correlation with spinal canal stenosis and spinal meningioma in the South Asian population, where the association between NO2 and spinal meningioma was more robust. As to East Asian population, NO2 was positively associated with trigeminal neuralgia (IVW: OR = 1.21, 95%CI: 1.02~1.43, P = 0.03), subarachnoid hemorrhage, pituitary adenoma and craniopharyngioma, focal brain injury, and negatively relevant to stroke and craniosynostosis, where the association between NO2 and subarachnoid hemorrhage was more robust. As to Greater Middle Eastern population, NO2 was positively associated with intracerebral hemorrhage, spinal canal stenosis, and negatively associated with malignant neoplasm of brain and other parts of CNS, where the relevance between NO2 and spinal canal stenosis was more robust. No causal correlation has been found between NO2 and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S6-S10).
3.4. Causal effects of PM2.5 on neurosurgical multisystem diseases
As for PM2.5, we discovered that PM2.5 was positively correlation with cerebral infarction in the European population, where the association was robust. As for African American or Afro-Caribbean population, PM2.5 was negatively associated with epilepsy, subarachnoid hemorrhage, and diffuse brain injury, where the association between PM2.5 and subarachnoid hemorrhage was more robust. As for South Asian population, PM2.5 was positively associated with congenital malformations of the nervous system. As for East Asian population, PM2.5 was negatively associated with cervical spondylosis, where the association was robust. As for Greater Middle Eastern population, PM2.5 was positively correlation with concussion, and negatively correlation with congenital malformations of the nervous system. No causal correlation has been discovered between PM2.5 and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S11-S15).
Causality of the risk for air pollution (NOx, NO2, PM2.5) in the world and Neurosurgical multisystem diseases outcomes (Positive result, p<0.05).
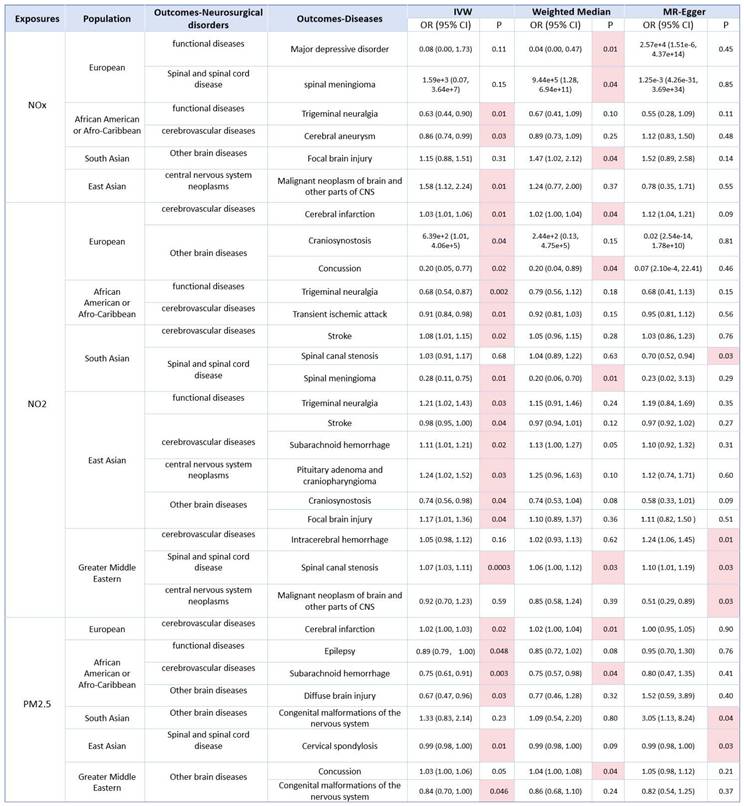
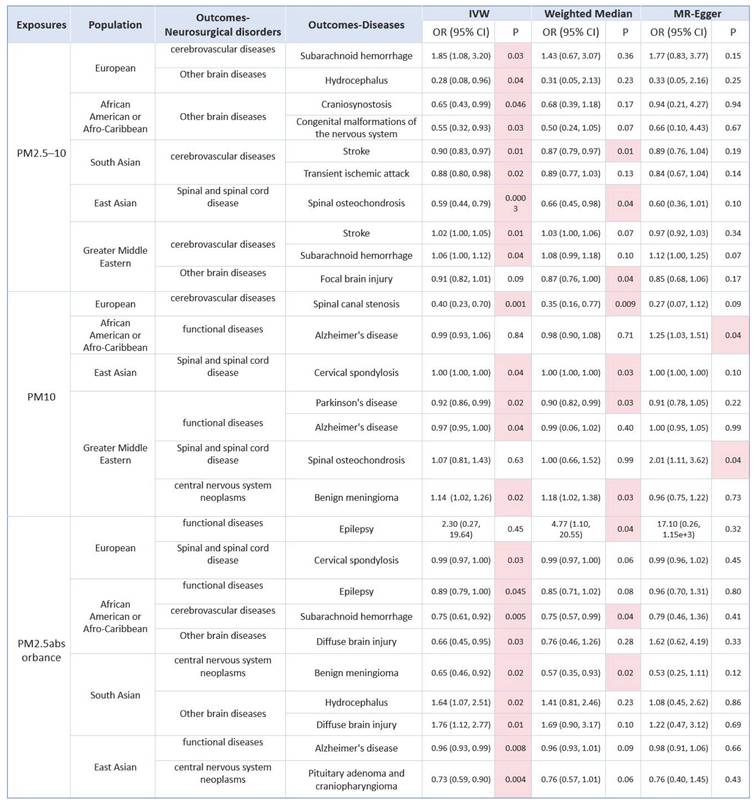
Causality of the risk for air pollution (PM2.5-10, PM10, PM2.5absorbance) in the world and Neurosurgical multisystem diseases outcomes (Positive result, p<0.05).
3.5. Causal effects of PM2.5-10 on neurosurgical multisystem diseases
As for PM2.5-10, we found that PM2.5-10 was positively correlation with subarachnoid hemorrhage, and negatively correlation with hydrocephalus in the European population. In African American or Afro-Caribbean population, PM2.5-10 was negatively associated with craniosynostosis and Congenital malformations of the nervous system. As for South Asian population, PM2.5-10 was negatively associated with stroke, and transient ischemic attack, where the association between PM2.5-10 and stroke was more robust. As for East Asian population, PM2.5-10 was negatively correlation with spinal osteochondrosis, where the correlation was robust. As to Greater Middle Eastern population, M2.5-10 was positively correlation with stroke and subarachnoid hemorrhage, and negatively correlation with focal brain injury. No causal correlation has been found between PM2.5-10 and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S16-S20).
3.6. Causal effects of PM10 on neurosurgical multisystem diseases
As for PM10, we found that PM10 was negatively associated with spinal canal stenosis in the European population, where the association was robust. As for African American or Afro-Caribbean population, PM10 was positively relevant to Alzheimer's disease. As for East Asian population, PM10 was positively associated with cervical spondylosis, where the association was robust. As to Greater Middle Eastern, we found that PM10 was negatively associated with Parkinson's disease and Alzheimer's disease, where the association between PM10 and Parkinson's disease was more robust. In addition, PM10 was positively associated with spinal osteochondrosis and benign meningioma, where the association between PM10 and benign meningioma was more robust. No causal correlation has been found between PM10 and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S21-S24).
3.7. Causal effects of PM2.5 absorbance on neurosurgical multisystem diseases
As for PM2.5 absorbance, we found that PM2.5 absorbance was positively correlation with epilepsy and negatively relevant to cervical spondylosis in the European population. As to African American or Afro-Caribbean population, PM2.5 absorbance was negatively associated with epilepsy, subarachnoid hemorrhage and diffuse brain injury, where the correlation between PM2.5 absorbance and subarachnoid hemorrhage was more robust. As for South Asian, PM2.5 absorbance was negatively relevant to benign meningioma, where the association was robust. Furthermore, PM2.5 absorbance was positively associated with hydrocephalus and diffuse brain injury. As for East Asian, we found that PM2.5 absorbance was negatively correlation with Alzheimer's disease and Pituitary adenoma and craniopharyngioma. No causal relevance has been found between PM2.5 absorbance and other neurosurgical disorders in other populations (Fig.3, Fig.4 and Table S25-S28).
3.8. Sensitivity analysis
Sensitivity analysis was used to weigh the dependability of the causal relevance between ambient air pollution and neurosurgical multisystem diseases. This analysis primarily comprised three components: heterogeneity, horizontal pleiotropy, and leave-one-out analysis. Heterogeneity was estimated via Cochran's Q test, P>0.05 manifesting no heterogeneity in the MR analysis. To guarantee the dependability of the conclusions, a random effects model was used for those with P<0.05. Additionally, the MR-Egger intercept was utilized to test for pleiotropy. P<0.05 represents pleiotropy, which showed results of the MR analysis are labile. The research indicates that instability occurs exclusively when there is a relevance between air pollution and neurosurgical diseases using the MR-Egger analysis method, whereas all other results remain robust (Table 2) (Table S29-S56). Overall, the sensitivity analysis conducted in this research corroborates the dependability of the given SNPs selected as genetic instruments, suggesting that air pollution constitutes a dangerous element for neurosurgical multisystem diseases.
4. Discussion
In recent years, ambient air pollution has emerged as an increasingly severe threat to human health, contributing to millions of premature deaths globally each year [39]. While numerous researches have extensively discovered the relevance between air pollution and the cardiovascular and respiratory systems [40, 41], there remains a paucity of systematic investigations into its causal association with neurosurgical multisystem diseases. Consequently, it is urgently imperative to search underlying risk elements and to develop effective preventive measures aimed at mitigating the disadvantageous health consequences of air pollution. Numerous prospective and observational researches have investigated the correlation between neurological diseases and air pollution across various racial groups. For instance, Ma et al. demonstrated that prolonged PM2.5 exposure is relevant to cognitive decline and an elevated dangerousness of Alzheimer's disease, attributed to amyloid accumulation in the brains of Chinese patients [5]. Conversely, Zhang et al. proceeded researches on the U.S. population and discovered no significant relevance between PM2.5 exposure and stroke. Furthermore, their findings indicated that stroke did not significantly alter or modulate the causal correlation between PM2.5 exposure and dementia [42]. In conclusion, the aforementioned studies did not systematically explore the correlation between air pollution and neurosurgical multisystem diseases, and their findings were devoid of genetic evidence. Consequently, this study tries to address this problem by exploring the potential genetic associations between six air pollution factors—namely PM2.5, PM2.5-10, PM10, PM2.5 absorbance, NO2 and NOx, and multiple neurological disorders.
Sensitivity analyses of MR-Egger intercept regression and Cochrane Q tests (Positive result).
| Exposures | Population | Outcomes-Neurosurgical disorders | Outcomes-Diseases | Q_MR.Egger | Q_df_MR.Egger | Q_pval | Q_IVW | Q_df_IVW | Q_pval | Egger_intercept | se | pval |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NOx | European | functional diseases | major depressive disorder | 11.11 | 4 | 0.03 | 14.26 | 5 | 0.01 | -0.1682 | 0.1582 | 0.3475 |
| spinal and spinal cord disease | spinal meningioma | 4.88 | 4 | 0.30 | 5.12 | 5 | 0.40 | 0.2027 | 0.4585 | 0.6812 | ||
| African American or Afro-Caribbean | functional diseases | trigeminal neuralgia | 6.38 | 15 | 0.97 | 6.61 | 16 | 0.98 | 0.0173 | 0.0361 | 0.6386 | |
| cerebrovascular diseases | cerebral aneurysm | 16.70 | 18 | 0.54 | 20.65 | 19 | 0.36 | -0.0331 | 0.0166 | 0.0624 | ||
| South Asian | other brain diseases | focal brain injury | 17.23 | 16 | 0.37 | 18.73 | 17 | 0.34 | -0.0366 | 0.0310 | 0.2544 | |
| East Asian | central nervous system neoplasms | malignant neoplasm of brain and other parts of cns | 3.69 | 8 | 0.88 | 7.50 | 9 | 0.58 | 0.1753 | 0.0896 | 0.0862 | |
| NO2 | European | cerebrovascular diseases | cerebral infarction | 1.67 | 2 | 0.43 | 6.84 | 3 | 0.08 | -0.0014 | 0.0006 | 0.1508 |
| other brain diseases | craniosynostosis | 0.16 | 2 | 0.92 | 0.73 | 3 | 0.87 | 0.1699 | 0.2244 | 0.5279 | ||
| other brain diseases | concussion | 0.59 | 2 | 0.74 | 0.73 | 3 | 0.87 | 0.175 | 0.0472 | 0.7466 | ||
| African American or Afro-Caribbean | functional diseases | trigeminal neuralgia | 15.33 | 25 | 0.93 | 15.33 | 26 | 0.95 | 0.0002 | 0.0271 | 0.9956 | |
| cerebrovascular diseases | transient ischemic attack | 20.36 | 25 | 0.73 | 20.79 | 26 | 0.75 | -0.0057 | 0.0086 | 0.5155 | ||
| South Asian | cerebrovascular diseases | stroke | 12.10 | 16 | 0.74 | 12.41 | 17 | 0.77 | 0.0041 | 0.0073 | 0.5857 | |
| spinal and spinal cord disease | spinal canal stenosis | 22.31 | 21 | 0.38 | 30.18 | 22 | 0.11 | 0.0341 | 0.0125 | 0.0128 | ||
| spinal and spinal cord disease | spinal meningioma | 10.36 | 18 | 0.92 | 10.38 | 19 | 0.94 | 0.0184 | 0.1102 | 0.8693 | ||
| East Asian | functional diseases | trigeminal neuralgia | 5.65 | 9 | 0.77 | 5.65 | 10 | 0.84 | 0.0035 | 0.0415 | 0.9355 | |
| cerebrovascular diseases | stroke | 9.14 | 10 | 0.52 | 9.24 | 11 | 0.60 | 0.0022 | 0.0069 | 0.7603 | ||
| cerebrovascular diseases | subarachnoid hemorrhage | 12.85 | 12 | 0.38 | 12.85 | 13 | 0.46 | 0.0010 | 0.0214 | 0.9640 | ||
| central nervous system neoplasms | pituitary adenoma and craniopharyngioma | 12.07 | 9 | 0.21 | 12.47 | 10 | 0.25 | 0.0273 | 0.0501 | 0.5986 | ||
| other brain diseases | craniosynostosis | 12.08 | 9 | 0.21 | 13.42 | 10 | 0.20 | 0.0673 | 0.0673 | 0.3437 | ||
| other brain diseases | focal brain injury | 8.54 | 9 | 0.48 | 8.68 | 10 | 0.56 | 0.0135 | 0.0362 | 0.7174 | ||
| Greater Middle Eastern | cerebrovascular diseases | intracerebral hemorrhage | 14.91 | 22 | 0.87 | 20.38 | 23 | 0.62 | -0.0515 | 0.0220 | 0.0289 | |
| spinal and spinal cord disease | spinal canal stenosis | 17.14 | 22 | 0.76 | 17.71 | 23 | 0.77 | -0.0085 | 0.0112 | 0.4576 | ||
| central nervous system neoplasms | malignant neoplasm of brain and other parts of cns | 18.56 | 18 | 0.42 | 24.40 | 19 | 0.18 | 0.1918 | 0.0806 | 0.0285 | ||
| PM2.5 | European | cerebrovascular diseases | cerebral infarction | 2.92 | 3 | 0.40 | 3.38 | 4 | 0.50 | 0.0002 | 0.0004 | 0.5486 |
| African American or Afro-Caribbean | functional diseases | epilepsy | 20.18 | 22 | 0.57 | 20.39 | 23 | 0.62 | -0.0061 | 0.0134 | 0.6543 | |
| cerebrovascular diseases | subarachnoid hemorrhage | 28.53 | 22 | 0.16 | 28.62 | 23 | 0.19 | -0.0061 | 0.0230 | 0.7916 | ||
| other brain diseases | diffuse brain injury | 19.83 | 21 | 0.53 | 23.20 | 22 | 0.39 | -0.0759 | 0.0414 | 0.0805 | ||
| South Asian | other brain diseases | congenital malformations of the nervous system | 19.82 | 24 | 0.71 | 23.26 | 25 | 0.56 | -0.0929 | 0.0501 | 0.0760 | |
| East Asian | spinal and spinal cord disease | cervical spondylosis | 11.42 | 11 | 0.41 | 13.37 | 12 | 0.34 | 0.0002 | 0.0001 | 0.1987 | |
| Greater Middle Eastern | other brain diseases | concussion | 15.63 | 26 | 0.94 | 15.91 | 27 | 0.95 | -0.0058 | 0.0110 | 0.6040 | |
| other brain diseases | congenital malformations of the nervous system | 20.45 | 26 | 0.77 | 20.46 | 27 | 0.81 | 0.0062 | 0.0663 | 0.9265 | ||
| PM2.5-10 | European | cerebrovascular diseases | subarachnoid hemorrhage | 39.77 | 39 | 0.44 | 39.80 | 40 | 0.48 | 0.0017 | 0.0094 | 0.8589 |
| other brain diseases | hydrocephalus | 32.60 | 36 | 0.63 | 32.65 | 37 | 0.67 | -0.0046 | 0.0199 | 0.8173 | ||
| African American or Afro-Caribbean | other brain diseases | craniosynostosis | 7.91 | 17 | 0.97 | 8.15 | 18 | 0.98 | -0.0403 | 0.0812 | 0.6265 | |
| other brain diseases | congenital malformations of the nervous system | 13.89 | 17 | 0.67 | 13.93 | 18 | 0.73 | -0.0203 | 0.1025 | 0.8451 | ||
| South Asian | cerebrovascular diseases | stroke | 8.28 | 8 | 0.41 | 8.30 | 9 | 0.50 | 0.0015 | 0.0098 | 0.8780 | |
| cerebrovascular diseases | transient ischemic attack | 3.77 | 10 | 0.96 | 4.07 | 11 | 0.97 | 0.0101 | 0.0183 | 0.5926 | ||
| East Asian | spinal and spinal cord disease | spinal osteochondrosis | 9.83 | 7 | 0.20 | 9.84 | 8 | 0.28 | -0.0085 | 0.0870 | 0.9247 | |
| Greater Middle Eastern | cerebrovascular diseases | stroke | 16.73 | 21 | 0.73 | 20.81 | 22 | 0.53 | 0.0129 | 0.0064 | 0.0562 | |
| cerebrovascular diseases | subarachnoid hemorrhage | 20.84 | 25 | 0.70 | 21.92 | 26 | 0.69 | -0.0167 | 0.0161 | 0.3093 | ||
| other brain diseases | focal brain injury | 34.69 | 23 | 0.06 | 35.40 | 24 | 0.06 | 0.0213 | 0.0312 | 0.5008 | ||
| PM10 | European | cerebrovascular diseases | spinal canal stenosis | 16.29 | 18 | 0.57 | 16.63 | 19 | 0.61 | 0.0080 | 0.0137 | 0.5650 |
| African American or Afro-Caribbean | functional diseases | alzheimer's disease | 7.90 | 12 | 0.79 | 13.83 | 13 | 0.39 | -0.0238 | 0.0098 | 0.0315 | |
| East Asian | spinal and spinal cord disease | cervical spondylosis | 3.18 | 8 | 0.92 | 4.30 | 9 | 0.89 | -0.0002 | 0.00002 | 0.3194 | |
| Greater Middle Eastern | functional diseases | parkinson's disease | 14.17 | 14 | 0.44 | 14.22 | 15 | 0.51 | 0.0043 | 0.0182 | 0.8176 | |
| functional diseases | alzheimer's disease | 17.73 | 14 | 0.22 | 19.47 | 15 | 0.19 | -0.0071 | 0.0060 | 0.2615 | ||
| spinal and spinal cord disease | spinal osteochondrosis | 12.04 | 14 | 0.60 | 17.48 | 15 | 0.29 | -0.1668 | 0.0715 | 0.0351 | ||
| central nervous system neoplasms | benign meningioma | 9.05 | 14 | 0.83 | 11.50 | 15 | 0.72 | 0.0453 | 0.0289 | 0.1396 | ||
| PM2.5absorbance | European | functional diseases | epilepsy | 5.97 | 2 | 0.05 | 9.43 | 3 | 0.02 | -0.0618 | 0.0574 | 0.3941 |
| spinal and spinal cord disease | cervical spondylosis | 0.18 | 2 | 0.91 | 0.19 | 3 | 0.98 | -0.0004 | 0.0003 | 0.9173 | ||
| African American or Afro-Caribbean | functional diseases | epilepsy | 20.00 | 21 | 0.52 | 20.28 | 22 | 0.57 | -0.0071 | 0.0136 | 0.6078 | |
| cerebrovascular diseases | subarachnoid hemorrhage | 28.45 | 21 | 0.13 | 28.51 | 22 | 0.16 | -0.0051 | 0.0238 | 0.8310 | ||
| other brain diseases | diffuse brain injury | 18.85 | 20 | 0.53 | 22.86 | 21 | 0.35 | -0.0847 | 0.0423 | 0.0590 | ||
| South Asian | central nervous system neoplasms | benign meningioma | 13.87 | 13 | 0.38 | 14.27 | 14 | 0.43 | 0.0244 | 0.0399 | 0.5524 | |
| other brain diseases | hydrocephalus | 4.14 | 13 | 0.99 | 5.25 | 14 | 0.98 | 0.0501 | 0.0478 | 0.3130 | ||
| other brain diseases | diffuse brain injury | 8.61 | 13 | 0.80 | 9.38 | 14 | 0.81 | 0.0448 | 0.0510 | 0.3957 | ||
| East Asian | functional diseases | alzheimer's disease | 7.06 | 9 | 0.63 | 7.52 | 10 | 0.68 | -0.0056 | 0.0082 | 0.5161 | |
| central nervous system neoplasms | pituitary adenoma and craniopharyngioma | 2.35 | 9 | 0.98 | 2.37 | 10 | 0.99 | -0.0106 | 0.0637 | 0.8720 |
This study is distinguished by several key aspects: 1. It presents the inaugural genetic evidence establishing a causal correlation between air pollution and neurosurgical multisystem disease; 2. It identifies specific variations in the impact of air pollution on neurological diseases across different racial and population groups; 3. It posits that a P-value of less than 0.05 in more than two distinct MR analyses indicates a robust correlation. The specific analysis results are as follows: 3.1. NO2 exposure is genetically predicted to significantly increase the risk of cerebral infarction in European populations, subarachnoid hemorrhage in East Asian populations, and Spinal canal stenosis in Greater Middle Eastern populations, while reducing the dangerousness of concussion in European populations and spinal meningioma in South Asian populations. 3.2. PM2.5 is a dangerousness element for cerebral infarction in European populations, and a protective factor for subarachnoid hemorrhage in African American or Afro-Caribbean populations and cervical spondylosis in East Asian populations. 3.3. PM2.5-10 exposure may be negatively related to stroke in South Asian populations and Spinal osteochondrosis in East Asian populations. 3.4. PM10 exposure may be positively associated with cervical spondylosis in East Asian populations and benign meningiomas in Greater Middle Eastern populations, but negatively associated with Spinal canal stenosis in European populations and Parkinson's disease in Greater Middle Eastern populations. 3.5. There may be a remarkable negative relevance between PM2.5 absorbance and subarachnoid hemorrhage in African American or Afro-Caribbean population and benign meningioma in South Asian population. 4. Air pollution is associated with the following diseases in more than two races and populations: 4.1. NO2: trigeminal neuralgia, stroke, spinal stenosis and craniosynostosis; 4.2. PM2.5: congenital malformations of the nervous system; 4.3. PM2.5-10: subarachnoid hemorrhage and stroke; 4.4. PM10: Alzheimer's Disease; 4.5. PM2.5 absorbance: epilepsy and diffuse brain injury. 5. From the perspective of different subspecialties of neurosurgery, the diseases associated with air pollution three or more times are as follows: 5.1. functional diseases: trigeminal neuralgia and epilepsy; 5.2. cerebrovascular diseases: stroke and subarachnoid hemorrhage; 5.3. spinal and spinal cord disease: spinal canal stenosis and cervical spondylosis; 5.4. other brain diseases: craniosynostosis, diffuse brain injury, focal brain injury and congenital malformations of the nervous system. 6. The following diseases were not found to be associated with air pollution: obsessive compulsive disorder, intracranial and intraspinal abscess, cervical spinal cord and nerve injuries, glioblastoma, malignant meningioma and benign neoplasm of brain and other parts of CNS.
Regarding functional diseases, this study identified a remarkable negative relevance between trigeminal neuralgia and exposure to NOx and NO2 within the African American or Afro-Caribbean population, while a positive association was observed with NO2 exposure in the East Asian population. Previous study on the correlation between trigeminal neuralgia and air pollution has not addressed the correlation with NOx and NO2, making this study the first to investigate this specific direction. Researchers in China identified no relevance between short-term air pollution exposure and epilepsy [43]. Conversely, a retrospective study conducted at a hospital indicated that air pollution, particularly elevated levels of PM2.5 and SO2, constitutes a risk factor for pediatric convulsions [44]. The current study elucidated that PM2.5 and PM2.5 absorbance are negatively relevant to African American or Afro-Caribbean populations from a genetic perspective. However, the mechanisms by which SNPs influence seizure susceptibility during pollutant exposure remain poorly understood, and there are notable racial disparities in the findings. For Parkinson's disease (PD), a retrospective study conducted by Korean researchers identified a strong relevance between NO2 exposure and the incidence and progression of Parkinson's disease (PD) [9]. In contrast, a study by Dutch researchers did not establish a remarkable relevance between air pollution exposure and the development of PD among local residents [45]. Our study indicates a remarkable relevance between PM10 exposure and the occurrence of PD in the Greater Middle Eastern population. These findings could inform the implementation of targeted public health interventions. Numerous researches have demonstrated that PM2.5 may elevate the incidence of Alzheimer's disease, potentially through mechanisms involving the reduction of DNA methylation levels, alterations in epigenetic regulation, damage to the CNS, and disruption of intestinal microecological balance [46]. The present study identifies a significant correlation between Alzheimer's disease and both PM10 and PM2.5 absorbance, thereby laying the groundwork for further investigation into the potential associations and underlying mechanisms linking this disease with air pollution.
Regarding cerebrovascular diseases, our study identified a remarkable relevance between NO2, PM2.5 and an elevated dangerousness of cerebral infarction in European populations. Notably, prior studies have not built a direct correlation between air pollution and cerebral infarction. Consequently, our findings offer novel insights into the etiology and progression of cerebral infarction, particularly within European cohorts. Additionally, existing literature suggests that air pollution exposure may heighten the dangerousness of ischemic stroke, especially among individuals with large artery and small vessel diseases. Short contact air pollution also enhances the risk of hemorrhagic stroke, but the effect of long-term exposure on hemorrhagic risk is unknown [12]. Our study identified that various air pollutants exert distinct effects across different ethnic groups. For example, elevated concentrations of NO2 were related to an increased dangerousness of stroke in South Asian populations, whereas the same pollutant appeared to have a protective effect in East Asian populations. The underlying mechanisms for these differential effects require further investigation. Hwang et al. demonstrated a significant relevance between air pollution and mortality due to subarachnoid hemorrhage, particularly among female patients. This heightened susceptibility in women may be attributed to their lower smoking rates compared to the general population, as well as anatomical and physiological differences such as smaller airway dimensions, increased airway reactivity, and greater deposition of particulate matter. [47]. Our research additionally identified a significant correlation between air pollution—specifically NO2, PM2.5, and PM2.5-10—and the incidence and progression of subarachnoid hemorrhage across nearly all ethnic groups.
Furthermore, we have, for the first time, elucidated a genetic basis for the causal relevance between air pollution and spinal cord diseases, including spinal stenosis and cervical spondylosis. This novel finding offers a foundational framework for future investigations into potential mechanisms and the formulation of preventive and control strategies.
Regarding central nervous system neoplasms, our consequences indicate a potential genetic relevance between air pollution and benign meningiomas. Specifically, we discovered a negative correlation between PM10 exposure and meningiomas in Greater Middle Eastern populations, and a positive relevance between PM2.5 exposure and meningiomas in South Asian populations. In contrast, Wu et al. conducted a cohort study on air pollution and benign brain tumors and found no remarkable relevance between air pollution and meningioma [48], This discrepancy may be attributed to factors such as racial differences and the limited sample size in their study, and our study was analyzed from a genetic perspective, which made it more credible and convincing. As for malignant brain tumors such as glioma, we have not yet found a genetic link between them and air pollution.
Regarding other neurological disorders, our study concentrated on the causal correlation between air pollution and craniosynostosis, as well as congenital malformations of the nervous system. Congenital malformations represent a significant reason of fetal death, infant mortality and morbidity [49]. Our consequences indicate a strong relevance between PM2.5, PM2.5-10 and congenital malformations of the central nervous system. This is in accordance with previous studies that have been thought have a strong association between PM10 exposure during the overall congenital malformations. Subsequent exposure to PM10 throughout pregnancy was associated with congenital heart disease, neurodevelopmental abnormalities, and tetralogy of Fallot. In contrast, PM2.5 and NO2 exposure was not relevant to congenital conditions or malformations [49]. Consequently, our study is the first to identify a relevance between PM2.5 and PM2.5-10 exposure and congenital malformations of the central nervous system, providing significant insights for disease prevention and control. As for craniosynostosis, we also reported it for the first time to provide ideas for follow-up work.
Air pollution has different impacts on the health of people in different regions, which may be caused by population stratification. Population stratification refers to the existence of subgroup structures (such as genetic background, socioeconomic status, race, etc.) in the study population, which leads to the distortion of exposure-disease associations [50]. In the study of air pollution, if the population in highly polluted areas also has other high-risk characteristics (such as poverty and poor medical conditions), it may wrongly attribute the health differences entirely to the pollution itself. Low-income areas are usually more polluted, but residents may also face higher stress, poorer diet and medical resources. These factors together exacerbate health risks [51]. Some genetic variations (such as GSTP1, TNF-α) may affect an individual's sensitivity to pollution. If the proportion of a specific ethnic group is high in a certain area, differences in "pollution resistance" may be observed [52].
Therefore, population stratification is an important source of deviation, but a comprehensive analysis needs to be conducted in combination with the characteristics of pollutants, climate and medical conditions. The future study design should give priority to controlling socioeconomic status, genetic background, or using instrumental variables (such as policy changes) to reduce confounding.
In this study, a comprehensive MR analysis was performed utilizing data from the GWAS database. The substantial sample size enhances the stability of the causal effect analysis and ensures consistency across various MR analytical methods. Additionally, the application of the MR-Egger analysis method augments the reliability and reproducibility of the investigation into the relevance between air pollution and multi-system diseases within the field of neurosurgery, while mitigating ethical concerns and research costs [53]. This study offers compelling genetic basis supporting the causal relevance between air pollution and neurosurgical multi-system diseases, thereby offering an innovative theoretical foundation for the prevention and cure of air pollution-induced neurological conditions. Notably, our study population encompasses data from ethnic groups across multiple regions, enhancing the comprehensiveness and rigor of our conclusions. Although the stabilized of our analysis, it is vital to realize the deficiencies of this study. Firstly, the exposure factors mainly selected in this study are PM2.5, PM2.5-10, PM10, PM2.5 absorbance, NO2 and NOx, so there is a lack of research on some specific air pollutants, such as O3, NO and SO2, so this study cannot provide more detailed analytical data to determine their impact on neurosurgical multisystem diseases. Furthermore, a fundamental assumption of MR analysis is the linear correlation between genetic variation, exposure factors, and outcomes. However, prior epidemiological studies indicate a nonlinear correlation between air pollution and disease [54]. Consequently, our study must rigorously account for potential nonlinear relationships or time-varying effects during the MR analysis. Despite certain drawbacks, our MR analysis yields valuable understandings into the genetic relevance between air pollution and neurosurgical multisystem disease. We believe that based on the consequences of this study, people will have a deeper insight of the underlying function of air pollution in neurological diseases in the future, so as to develop more effective prevention and control measures.
5. Recommendations for Future Investigations
Given the established causal correlation between ambient air pollution and neurosurgical multisystem diseases, several recommendations for future study are proposed. Firstly, it is imperative to elucidate the potential mechanisms through which air pollution interact with genetic elements, thereby increasing the dangerousness of neurosurgical multisystem diseases. This line of inquiry aims to identify and characterize the critical susceptibility windows for neurological diseases and to pinpoint underlying targets for intervention. Second, investigate the underlying interactions between air pollutants and genetic variants across different populations to determine whether specific genetic variants are more likely to be associated with particular neurological disorders. Third, as evidenced by this study, it is crucial to validate the causal correlation between air pollution and neurological diseases using data from multiple regions, ethnic groups, and datasets. Finally, large-scale prospective cohort studies will be essential to gather and monitor the long-term exposure of different populations to air pollution to build a more clearly causal correlation between exposure factors and outcomes in the future.
6. Conclusions
In conclusion, our study elucidates the environmental and societal ramifications of mitigating air pollution to diminish the dangerousness of multisystem diseases pertinent to neurosurgery. The implementation of robust air pollution prevention and cure way, the establishment of sustainable urban planning frameworks, the propelling of clean energy strategies, and the adoption of science-based occupational safeguards are pivotal in safeguarding public health. These consequences furnish critical evidence for policymakers, healthcare professionals, environmental organizations, and the general populace to advocate for and execute air quality enhancement initiatives on a global scale. Ultimately, it will benefit the whole world and improve human health.
Supplementary Material
Supplementary tables.
Acknowledgements
We appreciate the work of the open GWAS project and UK Biobank for their invaluable efforts.
Funding
This work was supported by the Foundation of Science and Technology Department of Sichuan Province (Grant No. 2022YFS0322 and 2024YFFK0058).
Author contributions
Lirui Dai: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing - original draft. Peizhi Zhou: Conceptualization, Supervision, Writing - review & editing. Shu Jiang: Conceptualization, Funding acquisition, Methodology, Writing - original draft.
Data availability
The original data are available in the open GWAS project (https://gwas.mrcieu.ac.uk/).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Guo P, Chen Y, Wu H. et al. Ambient air pollution and markers of fetal growth: A retrospective population-based cohort study of 2.57 million term singleton births in China. Environment international. 2020;135:105410
2. Liu C, Chen R, Sera F. et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. The New England journal of medicine. 2019;381(8):705-715
3. Louis S, Carlson AK, Suresh A. et al. Impacts of Climate Change and Air Pollution on Neurologic Health, Disease, and Practice: A Scoping Review. Neurology. 2023;100(10):474-483
4. Zeller M, Giroud M, Royer C. et al. Air pollution and cardiovascular and cerebrovascular disease: Epidemiologic data. Presse medicale. 2006;35(10 Pt 2):1517-1522
5. Ma YH, Chen HS, Liu C. et al. Association of Long-term Exposure to Ambient Air Pollution With Cognitive Decline and Alzheimer's Disease-Related Amyloidosis. Biological psychiatry. 2023;93(9):780-789
6. Chang KH, Teng CJ, Hsu YC. et al. Long-Term Exposure to Air Pollution Associates the Risk of Benign Brain Tumor: A Nationwide, Population-Based, Cohort Study in Taiwan. Toxics. 2022 10(4)
7. Li W, Wang W. Causal effects of exposure to ambient air pollution on cancer risk: Insights from genetic evidence. The Science of the total environment. 2024;912:168843
8. Gao X, Jiang M, Huang N. et al. Long-Term Air Pollution, Genetic Susceptibility, and the Risk of Depression and Anxiety: A Prospective Study in the UK Biobank Cohort. Environmental health perspectives. 2023;131(1):17002
9. Jo S, Kim YJ, Park KW. et al. Association of NO2 and Other Air Pollution Exposures With the Risk of Parkinson Disease. JAMA neurology. 2021;78(7):800-808
10. Wang J, Hu X, Yang T. et al. Ambient air pollution and the dynamic transitions of stroke and dementia: a population-based cohort study. EClinicalMedicine. 2024;67:102368
11. Wu G, Cai M, Wang C. et al. Ambient air pollution and incidence, progression to multimorbidity and death of hypertension, diabetes, and chronic kidney disease: A national prospective cohort. The Science of the total environment. 2023;881:163406
12. Verhoeven JI, Allach Y, Vaartjes ICH. et al. Ambient air pollution and the risk of ischaemic and haemorrhagic stroke. The Lancet Planetary health. 2021;5(8):e542-e552
13. Lee YG, Yoon SJ, Yoon SH. Air pollution is associated with faster cognitive decline in Alzheimer's disease. Annals of clinical and translational neurology. 2023;10(6):964-973
14. Murata H, Barnhill LM, Bronstein JM. Air Pollution and the Risk of Parkinson's Disease: A Review. Movement disorders: official journal of the Movement Disorder Society. 2022;37(5):894-904
15. Fernandes MJS, Carletti CO, Sierra de Araújo LF. et al. Respiratory gases, air pollution and epilepsy. Revue neurologique. 2019;175(10):604-613
16. Sekula P, Del Greco MF, Pattaro C. et al. Mendelian Randomization as an Approach to Assess Causality Using Observational Data. Journal of the American Society of Nephrology: JASN. 2016;27(11):3253-3265
17. Larsson SC, Butterworth AS, Burgess S. Mendelian randomization for cardiovascular diseases: principles and applications. European heart journal. 2023;44(47):4913-4924
18. Wang MH, Cordell HJ, Van Steen K. Statistical methods for genome-wide association studies. Seminars in cancer biology. 2019;55:53-60
19. Sudlow C, Gallacher J, Allen N. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS medicine. 2015;12(3):e1001779
20. Li Y, Yang Z. The causal effect of exposure to air pollution on risk of adverse pregnancy outcomes: A two-sample Mendelian randomisation study. The Science of the total environment. 2024;928:172234
21. Liu CX, Liu YB, Peng Y. et al. Causal effect of air pollution on the risk of cardiovascular and metabolic diseases and potential mediation by gut microbiota. The Science of the total environment. 2024;912:169418
22. Hu H, Yang X, Chen Q. et al. Causal association between air pollution and autoimmune diseases: a two-sample Mendelian randomization study. Frontiers in public health. 2024;12:1333811
23. Sun M, Gao M, Luo M. et al. Causal relationship between air pollution and chronic obstructive pulmonary disease in European and East Asian populations: a Mendelian randomization study. International journal of environmental health research. 2024:1-16
24. Li J, Liu Y, Lv H. et al. The causal relationship between long-term exposure to ambient fine particulate matter and cognitive performance: Insights from Mendelian randomization. Journal of hazardous materials. 2024;473:134659
25. Li Z, Wen J, Wu W. Causal relationship and shared genes between air pollutants and amyotrophic lateral sclerosis: A large-scale genetic analysis. CNS neuroscience & therapeutics. 2024;30(7):e14812
26. Skrivankova VW, Richmond RC, Woolf BAR. et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. Jama. 2021;326(16):1614-1621
27. VanderWeele TJ, Tchetgen Tchetgen EJ, Cornelis M. et al. Methodological challenges in mendelian randomization. Epidemiology (Cambridge, Mass). 2014;25(3):427-435
28. Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends in neurosciences. 2009;32(9):506-516
29. Lyon MS, Andrews SJ, Elsworth B. et al. The variant call format provides efficient and robust storage of GWAS summary statistics. Genome biology. 2021;22(1):32
30. Wang YY, Li Q, Guo Y. et al. Association of Long-term Exposure to Airborne Particulate Matter of 1 μm or Less With Preterm Birth in China. JAMA pediatrics. 2018;172(3):e174872
31. Cohen AJ, Brauer M, Burnett R. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet (London, England). 2017;389(10082):1907-1918
32. Zhao Y, Zhu Q, Lin J. et al. Association of Exposure to Particulate Matter Air Pollution With Semen Quality Among Men in China. JAMA network open. 2022;5(2):e2148684
33. Dai L, Lyu L, Zhou P. et al. Causal associations of COVID-19 on neurosurgical diseases risk: a Mendelian randomization study. Human genomics. 2024;18(1):13
34. Bowden J, Del Greco MF, Minelli C. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. International journal of epidemiology. 2016;45(6):1961-1974
35. Verbanck M, Chen CY, Neale B. et al. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nature genetics. 2018;50(5):693-698
36. Bowden J, Del Greco MF, Minelli C. et al. Improving the accuracy of two-sample summary-data Mendelian randomization: moving beyond the NOME assumption. International journal of epidemiology. 2019;48(3):728-742
37. Li J, Bai H, Qiao H. et al. Causal effects of COVID-19 on cancer risk: A Mendelian randomization study. Journal of medical virology. 2023;95(4):e28722
38. Li W, Huang M, Wang R. et al. Impact of genetically predicted atrial fibrillation on cancer risks: A large cardio-oncology Mendelian randomization study using UK biobank. Frontiers in cardiovascular medicine. 2022;9:974402
39. Miller MR, Newby DE. Air pollution and cardiovascular disease: car sick. Cardiovascular research. 2020;116(2):279-294
40. Bhatnagar A. Cardiovascular Effects of Particulate Air Pollution. Annual review of medicine. 2022;73:393-406
41. Vieceli T, Tejada S, Martinez-Reviejo R. et al. Impact of air pollution on respiratory microbiome: A narrative review. Intensive & critical care nursing. 2023;74:103336
42. Zhang B, Langa KM, Weuve J. et al. Hypertension and Stroke as Mediators of Air Pollution Exposure and Incident Dementia. JAMA network open. 2023;6(9):e2333470
43. Xu C, Fan YN, Kan HD. et al. The Novel Relationship between Urban Air Pollution and Epilepsy: A Time Series Study. PloS one. 2016;11(8):e0161992
44. Yang L, Sun L, Chu W. et al. Study of the Impact of Air Pollution on Convulsions in Children: A Hospital-Based Retrospective Study in Hangzhou, China. Clinical pediatrics. 2023;62(10):1186-1192
45. Toro R, Downward GS, van der Mark M. et al. Parkinson's disease and long-term exposure to outdoor air pollution: A matched case-control study in the Netherlands. Environment international. 2019;129:28-34
46. Shou Y, Huang Y, Zhu X. et al. A review of the possible associations between ambient PM2.5 exposures and the development of Alzheimer's disease. Ecotoxicology and environmental safety. 2019;174:344-352
47. Hwang J, Yi H, Jang M. et al. Air Pollution and Subarachnoid Hemorrhage Mortality: A Stronger Association in Women than in Men. Journal of stroke. 2022;24(3):429-432
48. Wu AH, Wu J, Tseng C. et al. Association Between Outdoor Air Pollution and Risk of Malignant and Benign Brain Tumors: The Multiethnic Cohort Study. JNCI cancer spectrum. 2020;4(2):pkz107
49. Feng Y, Liu X, Zhang X. et al. Global air pollution exposure and congenital anomalies: an updated systematic review and meta-analysis of epidemiological studies. International journal of environmental health research. 2024;34(5):2333-2352
50. Balmes JR. Household air pollution from domestic combustion of solid fuels and health. The Journal of allergy and clinical immunology. 2019;143(6):1979-1987
51. Landrigan PJ, Fuller R, Acosta NJR. et al. The Lancet Commission on pollution and health. Lancet (London, England). 2018;391(10119):462-512
52. Romieu I, Sienra-Monge JJ, Ramírez-Aguilar M. et al. Genetic polymorphism of GSTM1 and antioxidant supplementation influence lung function in relation to ozone exposure in asthmatic children in Mexico City. Thorax. 2004;59(1):8-10
53. Liu Y, Lai H, Zhang R. et al. Causal relationship between gastro-esophageal reflux disease and risk of lung cancer: insights from multivariable Mendelian randomization and mediation analysis. International journal of epidemiology. 2023;52(5):1435-1447
54. Pu H, Wang S, Wang Z. et al. Non-linear relations between life expectancy, socio-economic, and air pollution factors: a global assessment with spatial disparities. Environmental science and pollution research international. 2022;29(35):53306-53318
Author contact
![]() Corresponding author: Peizhi Zhou, Department of Neurosurgery, West China Hospital of Sichuan University, Sichuan University, Chengdu, Sichuan, China. Email: peizhizhounsedu.cn.
Corresponding author: Peizhi Zhou, Department of Neurosurgery, West China Hospital of Sichuan University, Sichuan University, Chengdu, Sichuan, China. Email: peizhizhounsedu.cn.

 Global reach, higher impact
Global reach, higher impact