Impact Factor
ISSN: 1449-1907
Int J Med Sci 2021; 18(5):1240-1246. doi:10.7150/ijms.53286 This issue Cite
Research Paper
Incidence and treatment of adult femoral fractures with osteogenesis imperfecta: An analysis of a center of 72 patients in Taiwan
1. Department of Pediatrics, MacKay Memorial Hospital, Hsinchu, Taiwan.
2. Institute of Clinical Medicine, National Yang-Ming University, Taipei, Taiwan.
3. Department of Orthopedics, MacKay Memorial Hospital, Taipei, Taiwan.
4. Department of Medicine, MacKay Medical College, New Taipei City, Taiwan.
5. Division of Genetics and Metabolism, Department of Medical Research, MacKay Memorial Hospital, Taipei, Taiwan.
6. College of Medicine, Fu-Jen Catholic University, Taipei, Taiwan.
7. Department of Pediatrics, MacKay Memorial Hospital, Taipei, Taiwan.
8. MacKay Junior College of Medicine, Nursing and Management, Taipei, Taiwan.
9. Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, Taiwan.
10. Department of Rare Disease Center, MacKay Memorial Hospital, Taipei, Taiwan.
11. Department of Infant and Child Care, National Taipei University of Nursing and Health Sciences, Taipei, Taiwan.
Received 2020-9-15; Accepted 2020-12-18; Published 2021-1-14
Abstract
Background: Osteogenesis imperfecta (OI) is a rare disease characterized by increased bone fragility and susceptibility for fractures. Only few studies have compared the management for femoral fractures in children with OI. Nevertheless, no cohort studies have described the treatment for femoral fractures in adults with OI in Taiwan. This study aimed to investigate and compare the incidence of union and non-union femoral fractures and the best treatment options to avoid non-union fractures.
Methods: We enrolled 72 patients with OI who were older than 18 years at MacKay Memorial Hospital between January 2010 and December 2018. Femoral fracture incidence, non-union rate, and treatment modality were analyzed.
Results: Of 72 patients with OI, 11 patients had femoral fractures and 4 patients of them had >1 femoral fracture. The incidence for all types of femoral fractures was 651 fractures per 100,000 person-years annually. In 15 total fractures, 4 fractures resulted in non-union, and patients with type 4 OI mostly had shaft fractures. The best outcomes for non-union shaft fracture is achieved by surgical treatment.
Conclusion: Adults with OI tended to develop femoral fractures and non-unions. Adults with type 4 OI were particularly at high risk for non-unions in shaft fractures with conservative treatment.
Keywords: adult, femoral fracture, non-union, osteogenesis imperfect, Taiwan
Introduction
Osteogenesis imperfecta (OI) is a rare connective tissue disease characterized by increased bone fragility and is also known as brittle bone disease. In addition, 90% of patients with OI have mutations in the COL1A1 or COL1A2 gene, which encodes for alpha-1 and alpha-2 chains in type 1 collagen [1]. Fractures and skeletal deformation are easily seen in patients with OI because bone tissue is mainly composed of type 1 collagen [2]. OI is also characterized by blue sclerae, dentinogenesis imperfecta, hyperlaxity, hearing loss, and short stature [3-5].
According to clinical variability and pattern of inheritance, Sillence classification has four OI types (types 1-4) (Table 1) [6]. Additional types have been added later, and type 5 is accepted worldwide. Type 1 is the mildest form of OI, and patients usually have blue sclerae and frequently have dentinogenesis imperfecta. Type 2 is a perinatal lethal form. Type 3 is the most severe (non-fatal) form of OI with multiple fractures, progressive deformity, and short stature. Patients are often wheelchair bound. Type 4 has a variable degree of deformity with normal sclerae. Patients with type 4 OI have increased fracture risk. The most frequent type in OI is type 1. Type 5 is characterized by mild to severe weak bones. Progressive calcifications of the interosseous membrane of forearm and lower leg are observed. Some patients also develop hyperplastic callus formation after fractures [3]. Bone fragility and fracture risk increase in the following order: Type 1 < Types 4, 5 < Type 3 < Type 2 [7].
Although femoral fractures are common in patients with OI, no studies have described the fracture and non-union incidence in adults due to the rarity of this disease [8-10]. The non-union rate in adults with OI is expected to be higher than that in non-adults with OI. Surgical treatment is more challenging due to anatomical and bone-related abnormalities [9, 11-13]. This study aimed to investigate the incidence of femoral fractures and non-unions in adults with OI and to review our experience on the best possible treatment for non-union fracture.
Methods
Participants
This retrospective study was conducted in the OI expert clinic for adults at MacKay Memorial Hospital, Taipei, Taiwan. Patients with OI with a femoral fracture at age 18 years or older were retrieved from January 2010 to December 2019. We excluded patients with an osseous primary tumor, metastatic disease, or prednisone use due to an increased fracture risk. Radiographs were taken due to recent bone fracture or localized pain, suggesting possible fracture. All patients (n=72) were confirmed the diagnoses by molecular analysis. Molecular diagnosis was performed using a combination of Sanger sequencing and targeted resequencing directed to scan the entire coding sequence. The publicly available databases DGV (Database of Genomic Variants), DECIPHER (Database of Chromosomal Imbalance and Phenotype in Humans Using Ensembl Resources), OMIM (Online Mendelian Inheritance in Man), PubMed, ClinVar and the UCSC Genome Browser were used to compare the present findings with previous reports and evaluate the morbidity of the candidate gene.
A new OI nomenclature combined with causative genes (A) Phenotypes with mild to moderate severity, (B) Progressively deforming and perinatally lethal phenotypes (Van Dijk FS, Sillence DO, 2014) (AD: autosomal dominant; AR: autosomal recessive; XL: X-linked recessive)
| OI syndrome names | Type | Gene | Locus | Protein product | Inheritance |
|---|---|---|---|---|---|
| (A) Non-deforming OI with blue sclerae | 1 | COL1A1 | 17q21.33 | Collagen alpha-1(I) chain | AD |
| COL1A2 | 7q22.3 | Collagen alpha-2(I) chain | AD | ||
| Common variable OI with normal sclerae | 4 | COL1A1 | 17q21.33 | Collagen alpha-1(I) chain | AD |
| COL1A2 | 7q22.3 | Collagen alpha-2(I) chain | AD | ||
| WNT1 | 12q13.12 | Wingless-type MMTV integration site family, member 1 | AD | ||
| CRTAP | 3p22.3 | Cartilage-associated protein (CRTAP) | AR | ||
| PPIB | 15q22.31 | Cyclophilin B (CyPB) | AR | ||
| SP7 | 12q13.13 | Osterix | AR | ||
| PLS3 | Xq23 | Plastin 3 | XL | ||
| OI with calcification in interosseous membranes | 5 | IFITM5 | 11p15.5 | Interferon-induced transmembrane protein 5 | AD |
| (B) Progressively deforming | 3 | COL1A1 | 17q21.33 | Collagen alpha-1(I) chain | AD |
| COL1A2 | 7q22.3 | Collagen alpha-2(I) chain | AD | ||
| BMP1 | 8p21.3 | Bone morphogenetic protein 1 | AR | ||
| CRTAP | 3p22.3 | Cartilage-associated protein (CRTAP) | AR | ||
| FKBP10 | 17q21.2 | Peptidyl-prolyl cis-transisomerase | AR | ||
| LEPRE1 | 1p34.2 | Prolyl 3-hydroxylase 1 (P3H1) | AR | ||
| PLOD2 | 3q24 | Procollagen-lysine, 2-oxoglutarate | AR | ||
| PPIB | 15q22.31 | 5-dioxygenase 2 | AR | ||
| SERPINF1 | 17p13.3 | Cyclophilin B (CyPB) | AR | ||
| SERPINH1 | 11q13.5 | Pigment-epithelium-derived factor (PEDF) | AR | ||
| TMEM38B | 9q31.1 | Heat shock protein 47 (HSP47) | AR | ||
| WNT1 | 12q13.12 | Trimeric intracellular cation channel B (TRIC-B) | AR | ||
| CREB3L1 | 11q11 | Wingless-type MMTV integration site family, member 1 | AR | ||
| Old Astrocyte | AR | ||||
| Specifically induced substance (OASIS) | AR | ||||
| Perinatally lethal OI | 2 | COL1A1 | 17q21.33 | Collagen alpha-1(I) chain | AD |
| COL1A2 | 7q22.3 | Collagen alpha-2(I) chain | AD | ||
| CRTAP | 3p22.3 | Cartilage-associated protein (CRTAP) | AR | ||
| LEPRE1 | 1p34.2 | Prolyl 3-hydroxylase 1 (P3H1) | AR | ||
| PPIB | 15q22.31 | Cyclophilin B (CyPB) | AR |
AO/OTA fracture and dislocation classification of femur (Meinberg EG, Agel J, Roberts CS, et al., 2018).
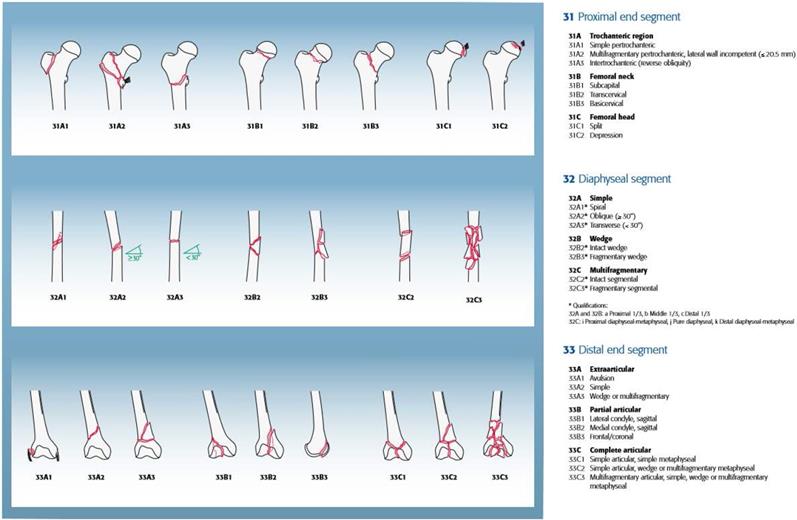
Besides demographic characteristics, we recorded the type of OI according to the Sillence classification. Femoral fractures were classified according to the AO/OTA Fracture and Dislocation Classification of Femoral Fractures (proximal, shaft, and distal, Figure 1) [14], type of treatment (intramedullary nailing [IN], plate fixation [PF], conservative) and outcome (union, non-union). Radiographic follow-up was used to determine union, defined as the presence of bridging callus in at least three of four cortices, which were evaluated on radiographs in two transverse levels [15]. Non-union was defined as non-radiographic changes to union or the absence of bridging callus of two or more cortices, which were evaluated on radiographs in two transverse levels, for at least 6 months after surgical or conservative treatment [16-17].
Statistical methods
A descriptive study was conducted because this study contains a relatively small number of subjects. Descriptive statistics were used to analyze the results using SPSS version 22.0 (SPSS, Inc., Chicago, IL). Categorical variables were expressed as percentage, and metric variables as mean and standard deviation.
Results
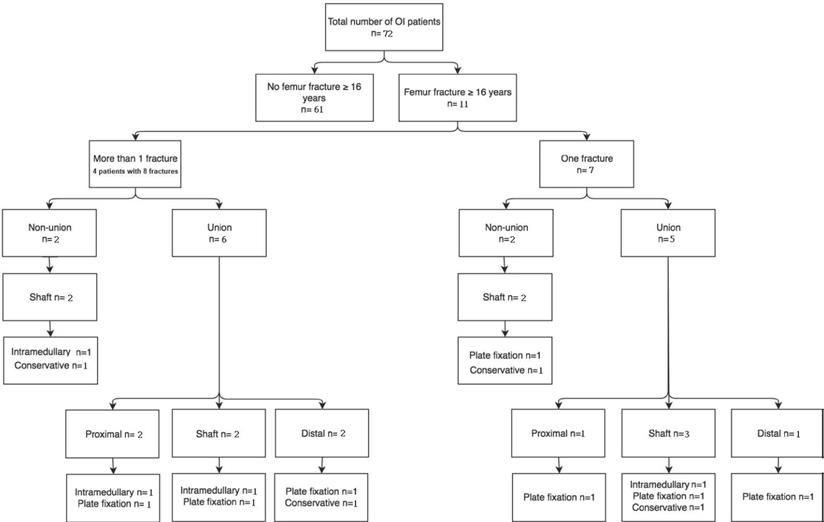
Table 2 shows the demographic characteristics of study subjects with OI. Subdivision of patients was based on the history of femoral fracture and, subsequently, history of non-union. Eleven (15.3%) patients had a femoral fracture (Figure 2). Four of these patients had more than one femoral fracture (total of eight fractures), resulting in 15 femoral fractures.
Influence of OI type on healing rate
Patients with OI types 3 and 4 were prone to femoral fractures; three (30.0%) and four (33.3%) of these patients with OI had at least one fracture. Of all patients with type 1 OI, four (8.0%) had one femoral fracture, and no patient had more than one femoral fracture. Of 15 femoral fractures, four fractures resulted in non-unions. All four non-unions were shaft fractures (Table 3; Figure 2).
Influence of treatment on healing rate
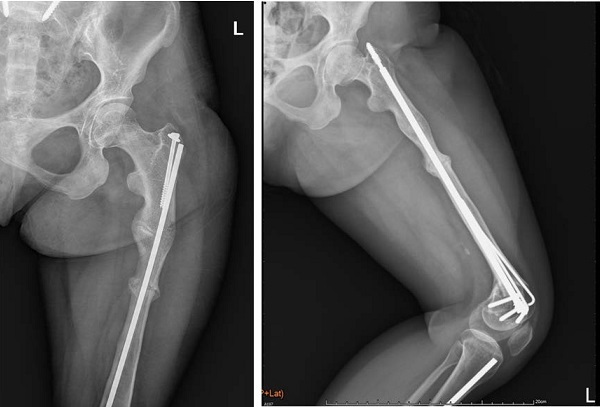
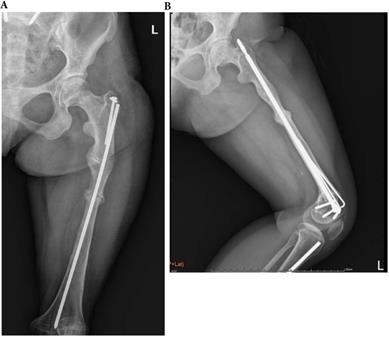
In OI type 4, 2 of 5 (40.0%) fractures resulted in non-union. All two patients with type 4 OI who were conservatively treated with OI had shaft fractures resulting in non-unions. Three other patients with type 4 were surgically treated for shaft fractures. All resulted in union (2 IN, 1 PF) (Figures 3, 4, 5). In patients with OI with type 1 OI, 1 of 4 (25.0%) fractures resulted in non-union (Figure 6), for type 3, 1 of 6 (16.7%) fractures resulted in non-union (Figure 7).
Flow diagram of fracture pattern and treatment.
A 33-year-old type 4 OI female suffered a left shaft femur fracture with plate fixation treatment in December 2015, resulting in union. (a) Just finished operation in December 2015 (b) Follow up in August 2016.

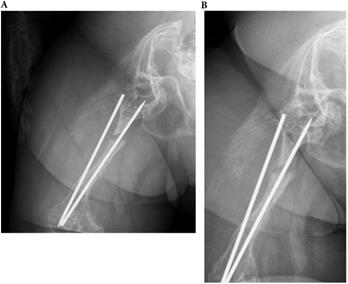
A 71-year-old female patients with type 4 OI had right midshaft femoral fracture with intramedullary nailing treatment in November 2014, which resulted in union. (a) Pre-operation fracture picture (b) Follow up in May 2016.

Overviewing all shaft fractures (n=9), intramedullary fixated fractures resulted in one non-union of three fractures (33.3%). Plate-fixated fractures resulted in one non-union of three fractures (33.3%). Conservatively treated shaft fractures resulted in two non-unions of three fractures (66.6%).
A 23-year-old female with type 4 OI had left distal femoral fracture with intramedullary nailing treatment in July 2016, which resulted in union. (a) Two weeks after operation (b) Follow up in July 2017.
Demographic characteristics of study subjects with osteogenesis imperfecta
| All patients (n = 72) | No femur fracture (n = 61) | Femur fracture (n = 11) | |
|---|---|---|---|
| Age (years) | 41.0 ± 15.3 | 40.4 ± 15.4 | 44.1 ± 14.7 |
| Gender (male, %) | 25 (34.7) | 20 (32.8) | 5 (45.5) |
| OI type (n, %) | |||
| 1 | 50 (69.4) | 45 (73.8) | 5 (45.5) |
| 2 | 0 (0.0) | ||
| 3 | 10 (13.9) | 8 (13.1) | 2 (18.2) |
| 4 | 12 (16.7) | 8 (13.1) | 4 (36.3) |
Data are presented as mean ± standard deviation or number of patients and percentages of group.
A 61-year-old type 4 OI female suffered a right midshaft femur fracture with intramedullary nailing treatment in August 2018, resulting in non-union. (a) Pre-operation fracture picture (b) Follow up in December 2019.

A 29-year-old type 3 OI female suffered a right shaft femur fracture with intramedullary nailing treatment in March 2012, resulting in non-union. (a) Just finished operation in March 2012 (b) Follow up in April 2013.
Patient characteristics comparing union and non-union groups in osteogenesis imperfecta, all femur fractures were included if age ≥18 years
| Union (n = 11) | Non-union (n = 4) | |
|---|---|---|
| Age (years) | 44.9±14.4 | 45.5±13.1 |
| Age at fracture (years) | 36.3±13.0 | 40.1±13.1 |
| Gender (male, %) | 6 (54.5) | 1 (25.0) |
| OI type (n, %) | ||
| 1 | 3 (27.3) | 1 (25.0) |
| 2 | 0 (0.0) | 0 (0.0) |
| 3 | 5 (45.4) | 1 (25.0) |
| 4 | 3 (27.3) | 2 (50.0) |
| Type of fracture (n, %) | ||
| Proximal | 3 (27.3) | 0 (0.0) |
| Shaft | 5 (45.4) | 4 (100.0) |
| Distal | 3 (27.3) | 0 (0.0) |
| Type of treatment (n, %) | ||
| Plate fixation | 6 (54.5) | 1 (25.0) |
| Intramedullary fixation | 3 (27.3) | 1 (25.0) |
| Conservative | 2 (18.2) | 2 (50.0) |
Data are presented as mean ± standard deviation or number of patients and percentages of group.
Discussion
In this study, we reviewed 72 adult patients with OI with or without femoral fractures and unions or non-unions. Eleven patients had 15 femoral fractures (15.3%) and 4 non-unions (26.7%). Adults with type 4 OI tended to develop non-unions by conservative treatment for midshaft fractures similar to a previous study [18]. For all types of femoral fractures, the incidence was 651 fractures per 100,000 person-years annually. The incidence was 355 fractures per 100,000 and 10 per 100,000 person-years annually for shaft fractures and femoral shaft fractures, respectively [19-20]. These results reveal a convincing discrepancy that patients with OI have more femoral fractures than patients with non-OI.
This is the first study describing the incidence and non-union rate of femoral fractures in adults with OI in Taiwan. Some smaller studies compared outcomes between different treatments in children with OI. Chiarello et al. compared the outcomes between surgical and conservative treatments of 29 children with long bone fragility fractures. They reported a slightly lower non-union and delayed-union rates under surgical treatment [21]. Enright and Noonan described femoral and tibial fractures with bone plating in four children with type 3 OI, which resulted in high complication rates [22]. Agarwal and Joseph and Gamble et al. found a 15%-20% prevalence on non-union fracture in a heterogeneous group of children with OI over a 10-14-year period [23-24]. However, the number of patients is small, and the results could not be extrapolated to adults, whereas it is 7.3 times higher non-union rate compared with adults with non-OI than in children with non-OI [25].
Limitations
Although our study revealed new insights on the incidence of femoral fractures and non-union in adults with OI, it also has limitations in analyzing for non-union. There are many causative factors for non-union, including bisphosphonate use, DXA scans, smoking status, nutritional deficiency, vitamin D deficiency, mobilization status, metabolic disease, or endocrine pathology [26]. We were unable to adjust these confounders due to lost data of these factors. Furthermore, 34 patients (47.2%) received bisphosphonate treatment after the diagnosis of OI in our study and all patients with femur fractures using bisphosphonate. It might cause that non-union fractures turn to union fractures even if under conservative treatment. Additionally, in our patients with femur fractures (n=11), 9 patients had femoral implants (nail or plate) before the diagnosis of OI. This may influence the number of fractures in adult life. Moreover, we also needed more patients' data to strengthen the results due to the limited number of fractures.
Recommendations for shaft fractures
Although this study has its limitations, we could state that adults with OI have a high tendency for non-unions with conservative treatment in femoral shaft fractures. We recommend surgical treatment for shaft fractures according to our data. We suggest intramedullary nailing in the surgical treatment for femoral shaft fractures despite the fact that our study results in no definite consensus. Intramedullary nailing is the standard treatment for femoral shaft fracture in adults with non-OI. Its advantages include optimal mechanical stability, efficient load transfer, minimization of stress concentration, early mobilization of hip and knee, preservation of soft tissues, fracture hematoma, and periosteal blood supply [17, 27-29]. Karadimas et al. reviewed the complications of intramedullary nails in non-OI femoral fracture. They reported a non-union rate of 1%-14.1% [30]. Excluding the study by Noumi et al., which only included open fractures, the non-union rates decreased to 1%-7.6% [31-32]. We could use a smaller nail in cases with anatomical abnormalities. It is also practical to use a humeral nail in cases of narrow intramedullary canal with a wedge osteotomy, if necessary. Patients' care should be personalized based on their characteristics, type of fracture, anatomical situation, and pre-existent materials. Caring for these patients with centralization and multidisciplinary work-up is needed (orthopedic surgeon, anesthetist, rehabilitation specialist, physiotherapist, occupational therapist, internist, geneticist, and radiologist).
Conclusion
In conclusion, adult patients with OI had a high incidence of femoral fractures and non-union rates. Conservative treatment in femoral shaft fractures in adults with OI had a high tendency for non-unions, particularly for patients with type 4 OI, probably because determining the severity of fracture in patients with type 4 OI is difficult for physicians, and they would hesitate to treat patients by conservative or surgical treatment. This study provides valuable features of a unique collection of patients with OI. However, confounding factors were not analyzed, and larger cohort studies are needed to determine the best treatment for femoral fractures in adult patients with OI.
Acknowledgements
We acknowledge the participation of study patients and their families. This study was supported by research grants from the Ministry of Science and Technology, Executive Yuan, Taiwan (MOST-109-2314-B-195-024, MOST-108-2314-B-195-012, MOST-108-2314-B-195-014, MOST-106-2314-B-195-015-MY2, and MOST-105-2628-B-195-001-MY3) and MacKay Memorial Hospital (MMH-E-109-16, MMH-E-108-16, MMH-MM-10801, and MMH-107-82).
Authorship statement
CLL, HYL and SPL conceived and planned the project; CLL wrote the manuscript with contributions from SCL, CYY, HYL and SPL; SCL, CYY, HYL and SPL examined all the cases; CLL and CKC collated and analyzed the clinical data. This manuscript has not been submitted to, nor is under review at, another journal or other publishing venue.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Van Dijk FS, Byers PH, Dalgleish R. et al. EMQN best practice guidelines for the laboratory diagnosis of osteogenesis imperfecta. Eur J Hum Genet. 2012;20:11-9
2. Fratzl-Zelman N, Misof BM, Klaushofer K. et al. Bone mass and mineralization in osteogenesis imperfecta. Wien Med Wochenschr. 2015;165:271-7
3. Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004;363:1377-85
4. Lin HY, Lin SP, Chuang CK. et al. Clinical features of osteogenesis imperfecta in Taiwan. J Formos Med Assoc. 2009;108(7):570-6
5. Lin HY, Chuang CK, Su YN. et al. Genotype and phenotype analysis of Taiwanese patients with osteogenesis imperfecta. Orphanet J Rare Dis. 2015;10:152
6. Van Dijk FS, Sillence DO. Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A. 2014;164:1470-81
7. Glorieux FH. Osteogenesis imperfecta. Best Pract Res Clin Rheumatol. 2008;22:85-100
8. Mulpuri K, Joseph B. Intramedullary rodding in osteogenesis imperfecta. J Pediatr Orthop. 2000;20:267-73
9. Nicolaou N, Agrawal Y, Padman M. et al. Changing pattern of femoral fractures in osteogenesis imperfecta with prolonged use of bisphosphonates. J Child Orthop. 2012;6:21-7
10. Chow W, Negandhi R, Kuong E. et al. Management pitfalls of fractured neck of femur in osteogenesis imperfecta. J Child Orthop. 2013;7:195-203
11. Meier RPH, Lorenzini KI, Uebelhart B. et al. Atypical femoral fracture following bisphosphonate treatment in a woman with osteogenesis imperfecta - a case report. Acta Orthop. 2012;83:548-50
12. Reyes C, Hitz M, Prieto-Alhambra D. et al. Risks and benefits of bisphosphonate therapies. J Cell Biochem. 2016;117:20-8
13. Lin HY, Lin SP, Chuang CK. et al. Intravenous pamidronate therapy in Taiwanese patients with osteogenesis imperfecta. Pediatr Neonato. 2008;49(5):161-5
14. Meinberg EG, Agel J, Roberts CS. et al. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32( Suppl 1):1-170
15. Den Boer FC, Patka P, Bakker FC. et al. Current concepts of fracture healing, delayed unions, and nonunions. Osteo Trauma Care. 2002;10:1-7
16. Frölke JPM, Patka P. Definition and classification of fracture nonunions. Int J Care Injured. 2007;38:19-22
17. Cleveland KB. Delayed union and nonunion of fractures. In: Campbell's operative orthopaedics, 12th edn. Philadelphia. 2013 p:2981-3016
18. Goudriaan WA, Harsevoort GJ, van Leeuwen M. et al. Incidence and treatment of femur fractures in adults with osteogenesis imperfecta: an analysis of an expert clinic of 216 patients. Eur J Trauma Emerg Surg. 2020;46(1):165-171
19. Salminen ST, Pihlajamaki HK, Avikainen VJ. et al. Population based epidemiologic and morphologic study of femoral shaft fractures. Clin Orthop Relat Res. 2000;372:241-9
20. Singer BR, McLauchlan GJ, Robinson CM. et al. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Jt Surg Br. 1998;80:243-8
21. Chiarello E, Donati D, Tedesco G. et al. Conservative versus surgical treatment of osteogenesis imperfecta: a retrospective analysis of 29 patients. Clin Cases Min Bone Metab. 2012;9:191-4
22. Enright WJ, Noonan KJ. Bone plating in patients with type III osteogenesis imperfecta: results and complications. Iowa Orthop J. 2006;26:37-40
23. Agarwal V, Joseph B. Non-union in osteogenesis imperfecta. J Pediatr Orthop. 2005;14:451-5
24. Gamble JG. Rinsky LA, Strudwick J, et al. Non-union of fractures in children who have osteogenesis imperfecta. J Bone Jt Surg Am. 1988;80:439-43
25. Mills LA, Simpson AH. The risk of non-union per fracture in children. J Child Orthop. 2013;7:317-22
26. Niikura T, Lee SY, Sakai Y. et al. Causative factors of fracture nonunion: the proportions of mechanical, biological, patient-dependent, and patient-independent factors. J Orthop Sci. 2014;19:120-4
27. Papakostidis C, Psyllakis I, Vardakas D. et al. Femoral-shaft fractures and nonunions treated with intramedullary nails: the role of dynamisation. Int J Care Inj. 2011;42:1353-61
28. Wolinsky PR, McCarty E, Shyr Y. et al. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46:392-9
29. Metsemakers WJ, Roels N, Belmans A. et al. Risk factors for nonunion after intramedullary nailing of femoral shaft fractures: remaining controversies. Int J Care Inj. 2015;46:1601-7
30. Karadimas EJ, Papadimitriou G, Theodoratos G. et al. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strat Traum Limb Reconstr. 2009;4:113-21
31. Noumi T, Yokoyama K, Ohtsuka H. et al. Intramedullary nailing for open fractures of the femoral shaft: evaluation of contributing factors on deep infection and nonunion using multivariate analysis. Int J Care Inj. 2005;36:1085-93
32. Santolini E, West R, Giannoudis PV. Risk factors for long bone fracture non-union: a stratification approach based on the level of the existing scientific evidence. Int J Care Inj. 2015;46:8-19
Author contact
![]() Corresponding authors: Hsiang-Yu Lin, Department of Pediatrics, MacKay Memorial Hospital, No.92, Sec. 2, Chung-Shan North Road, Taipei 10449, Taiwan. Fax: +886-2-2543-3642 and +886-2-2543-3535 ext. 3080. Shuan-Pei Lin, Department of Pediatrics, MacKay Memorial Hospital, No.92, Sec. 2, Chung-Shan North Road, Taipei 10449, Taiwan. Fax: +886-2-2543-3642 and +886-2-2543-3535 ext. 3080. E-mail: lxc46199hinet.net (H.-Y. Lin); 4535lincom (S.-P. Lin).
Corresponding authors: Hsiang-Yu Lin, Department of Pediatrics, MacKay Memorial Hospital, No.92, Sec. 2, Chung-Shan North Road, Taipei 10449, Taiwan. Fax: +886-2-2543-3642 and +886-2-2543-3535 ext. 3080. Shuan-Pei Lin, Department of Pediatrics, MacKay Memorial Hospital, No.92, Sec. 2, Chung-Shan North Road, Taipei 10449, Taiwan. Fax: +886-2-2543-3642 and +886-2-2543-3535 ext. 3080. E-mail: lxc46199hinet.net (H.-Y. Lin); 4535lincom (S.-P. Lin).

 Global reach, higher impact
Global reach, higher impact