3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2011; 8(2):156-160. doi:10.7150/ijms.8.156 This issue Cite
Research Paper
Efficacy of the Valsalva Maneuver on Needle Projection Pain and Hemodynamic Responses During Spinal Puncture
Department of Anesthesiology, Tehran University of Medical Sciences, Dr Shariati Hospital, TEHRAN, IRAN
Received 2010-10-24; Accepted 2011-2-8; Published 2011-2-16
Abstract
This study evaluated the efficacy of the valsalva maneuver that can induce baroreceptor activation and nociception, on needle projection pain and hemodynamic responses associated with spinal puncture. Ninety adults, ASA physical status I and II undergoing elective surgeries were included. Patients were randomized into three equal groups. Group I (C): control; Group II (B): ball; pressed a rubber ball (attention-diverting method); Group III (V): valsalva; blew into sphygmomanometer tubing and hold the mercury column up to 30 mm Hg for a period of at least 20s. Spinal needle projection pain was graded using numeric rating scale (NRS): 1-10, where scales of 1-3 were rated as mild, 4-6 as moderate, and > 6 as severe. Blood pressure and heart rate, five minutes before the procedure, during the spinal puncture and first and third minutes after that, were also recorded. Significant reduction in NRS was observed in the valsalva group compared with the control and the ball groups (p=0.001). There were statistical but no significant clinical differences in mean arterial blood pressure and heart rates between the study groups (P=0.008 and P=0.016 respectively). In conclusion valsalva maneuver can decrease the skin puncture pain associated with spinal needle projection while observing hemodynamic changes.
Keywords: Hemodynamic response, Lumbar puncture, Pain, Spinal anesthesia, Valsalva maneuver.
Introduction
Spinal anesthesia is a simple and reliable method of anesthetizing lower part of body. However many people refuse it because of fear of needle and back pain.1
Many techniques have been used to obtund pain of needle insertion including infiltration analgesia and EMLA patch. Local anesthetics themselves may produce pain on injection and many anesthetists are unsure that infiltration analgesia at the site of spinal puncture has any advantage over a straightforward puncture without analgesia. 2, 3, 4
The pain experienced during spinal puncture has both somatic and psychological components. Pharmacological measures, such as the application of local anesthetics, treat only the somatic component of pain, whereas attention-diverting measures (pressing ball) address only the psychological component of pain. 4, 5, 6
A literature search revealed laboratory studies showing that baroreceptor activation induces nociception but there were few clinical studies exploring the effect of the Valsalva maneuver on pain.6-10
In a study by Agrawal et al, Valsalva maneuver performed before venous canulation could decrease the incidence and severity of pain associated with venipuncture in adult patients.7
In another study by Gupta et al the efficacy of balloon inflation were evaluated on venipuncture pain in children aged 6-12 year and there was a significant reduction of pain in balloon group compared with distraction and control groups.8
This study evaluated the efficacy of Valsalva maneuver on needle projection pain and hemodynamic responses during spinal puncture.
Methods and Materials
This randomized clinical trial was performed in Dr.Shariati Hospital of Tehran University of Medical Sciences from January to March 2010. The study protocol conformed to the ethical guidelines of the 1989 Declaration of Helsinki.
Ethics Statement
To evaluate the effect of valsalva maneuver on pain, first, we searched Medline, ISI, and other databases. This intervention was noninvasive and previous studies reported that baroreceptor activation induces nociception. This trial was then registered with and approved by the Research Ethics Committee of Tehran University of Medical Sciences and Iranian Registry of Clinical Trials. Patients were instructed about the procedure and informed consent was obtained separately before surgery.
Participants and measurements
Ninety consecutive adults' patients, either sex with ASA physical status I and II, scheduled for elective surgeries under spinal anesthesia, were included. Patients having problems in communication, any contraindications to spinal anesthesia and Patients who could not hold the mercury column up to 30 mm Hg for a period of at least 20s and whose spinal puncture could not be performed in the first attempt were excluded.
Using a computer-generated randomization list, Patients were allocated into three equal groups. Group I (C): control; Group II (B): ball; pressed a rubber ball (attention-diverting method); Group III (V): valsalva; blew into sphygmomanometer tubing and hold the mercury column up to 30 mm Hg for a period of at least 20s.
Spinal needle projection pain was graded using numeric rating scale (NRS): 1-10, where scales of 1 -3 were rated as mild, 4-6 as moderate, and > 6 as severe pain.
In a pilot study of 20 patients having spinal anesthesia by 25-guage Quincke needle without introducer and any local infiltration, 90% of them had moderate to severe pain using NRS and nobody had NRS=0 (unpublished observation). According to this pilot study the NRS was graded from 1 to 10.
Before the surgery, patients were instructed about the Numeric Rating Scale (NRS) and how to blow into sphygmomanometer tubing.
All patients were premedicated with 10 mg diazepam given orally on the morning of surgery. On arrival in the operating room, ECG electrodes and non-invasive blood pressure (NIBP) monitor were applied and oxygen saturation was monitored by pulse oxymeter.
Patients were hydrated with 5ml.kg-1 ringer lactate solution. Spinal anesthesia was performed in lateral position by 25-guage Quincke needle without introducer.
The puncture pain was assessed by the patients, immediately after being placed supine for surgery using numeric rating scale (NRS).
Blood pressure and heart rate five minutes before the procedure, during spinal puncture and first and third minutes after that were also recorded.
Statistical analysis
In a pilot study of 20 patients having spinal anesthesia by 25-guage Quincke needle, 90% of them had moderate to severe pain using NRS (unpublished observation). Presuming that valsalva maneuver during spinal needle projection would reduce pain to 50%; one would need to enroll 30 patients in each group for the results to be statistically significant at a power of 95% with a level of confidence of 5%. Data were analyzed by SPSS version 11.5(SPSS Inc., Chicago, IL). Normality of distribution was tested by Kolmogorov Smirnov test. One-way ANOVA, Kruskal Wallis, Chi-square and Fishers exact tests were used when appropriate. Repeated measures ANOVA and post Hoc Tukey tests were used for comparing hemodynamic responses between the study groups. P<0.05 was considered statistically significant.
Results
There were no statistical differences in the demographic data between the study groups (P>0.05) (Table 1).
A significant reduction in NRS was observed in the valsalva group compared with the control and the ball groups (p=0.001) (Table 2).
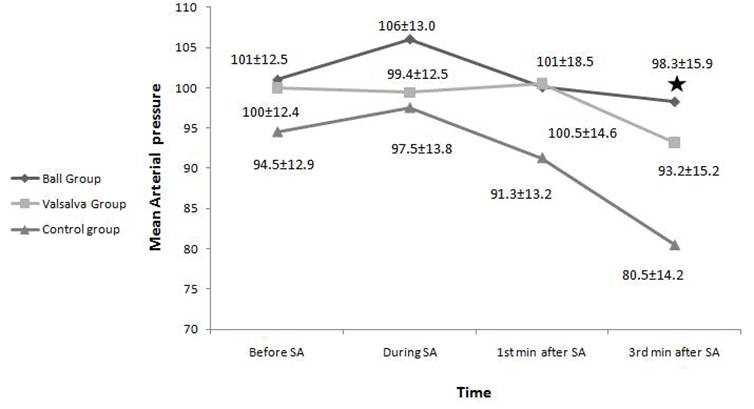
The mean arterial pressure (MAP) throughout the time intervals of prespinal procedure to the third minutes after that were statistically different between the study groups (P= 0.008).
Post Hoc Tukey test showed there was statistical difference in MAP between the ball and the control groups at third minutes after spinal anesthesia (p=0.007) (Fig 1).
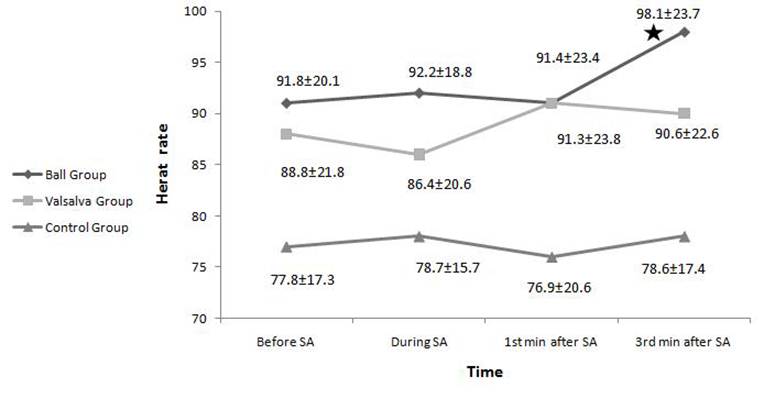
The mean heart rate (HR) throughout the time intervals of prespinal to the third minutes after that were statistically different between the study groups (P= 0.016).
Post Hoc Tukey test showed there was statistical difference in HR between the ball and the control groups at third minutes after spinal anesthesia (p=0.003) (Fig 2).
Comparing demographic data between the study groups.
| Variable | Group I(Control) N=30 | Group II(Ball) N=30 | Group III(Valsalva) N=30 |
|---|---|---|---|
| Age (year)a | 31.9±8.4 | 38.5±19.4 | 39.2±12.5 |
| Sex (M/F) | 15/15 | 19/11 | 20/10 |
| ASA Class (I/II) | 26/4 | 22/8 | 22/8 |
| Weight (Kg)a | 75.0±12.6 | 70.2±5.9 | 68.8±11.2 |
a: Data are presented as mean ± SD
There were no significant statistical differences between the study groups, P>0.05
Severity of spinal needle projection pain in the study groups
| Severity of pain (NRS)a | Group I(control) (N=30) | Group II(ball) (N=30) | Group III(valsalva) (N=30) |
|---|---|---|---|
| Mild (1-3) Moderate (4-6) Sever (7-10) | 9(30%) 19(63.3%) 2(6.7%) | 6(20%) 24(80%) 0(0%) | 21(70%) 9(30%) 0(0%) |
Data are presented as number (percent) of patients
Fisher exact test, P<0.001 between study groups
a: NRS= numeric rating scale
Comparing mean arterial blood pressure between the study groups five minute before spinal anesthesia (SA), during the procedure and first and third minutes after that, P = 0.008 between the study groups.
Comparing heart rate (HR) between the study groups five minute before spinal anesthesia (SA), during the procedure and first and third minutes after that( P=0.016 between the study groups).
Discussion
This study suggests that performing Valsalva maneuver during spinal needle projection reduces the severity of spinal needle puncture pain.
During valsalva maneuver intrathoracic pressure increases. This increase results in compression of the vessels within the chest and in turn results in baroreceptor activation. Activation of either the cardiopulmonary baroreceptor reflex arc or the sinoaortic baroreceptor reflex arc induces antinociception.9,10
There were few studies for evaluating the efficacy of balloon inflation on venipuncture pain in pediatric and adult patients.
In a study by Gupta et al on seventy-five pediatric patients aged 6-12 yr, the efficacy of balloon inflation for attenuating venipuncture pain was evaluated. Pain was self-reported by a pain face scale with a 10-cm visual analog scale (VAS) placed at its back, where 0=“no pain” and 10 = “worst imaginable pain”. VAS scores of 1- 3 were rated as mild, 4-6 as moderate, and 6 as severe.
Median (interquartile range) VAS score in the balloon group was 1 (3), which was reduced as compared with 2 (2) and 4 (2) observed in the distraction and control groups respectively (p= 0.000). Significant reduction in the incidence and severity of venipuncture pain was also observed in the balloon group compared with the other 2 groups (p<0.05).These findings were correlated with our study.
In another study by Agrawal et al, the efficacy of the Valsalva maneuver on pain associated with venous canulation were evaluated on Seventy-five adults patients undergoing elective surgeries. They were randomized into three groups of 25 each. Group I (C): control; Group II (V): blew into sphygmomanometer tubing and raised the mercury column up to 30mmHgfor 20 s; Group III (B): pressed a rubber ball. Twenty seconds later, peripheral venous canulation was performed. Venous canulation pain was graded using a 4-point scale: 0-3, where 0= no pain, 1= mild pain, 2= moderate pain and 3= severe pain, and visual analog scale of 0-10, where 0=no pain and 10= worst imaginable pain.
Agrawal et al used both, 4-point scale and VAS, in which the first scaling was used during the canulation and VAS was used after the canulation. They found a significant reduction in the incidence of pain in the Valsalva group: 18 of 25 (72%) patients, whereas 25 of 25 (100%) experienced pain in the other two groups (p<0.001). These findings were also correlated with our study.
In our study, only 9(30%) of patients had moderate and severe pain in valsalva group, where 24 (80%) in ball group and 21 (70%) in control group had moderate and sever pain.
Since Valsalva maneuver may induce Bradycardia and hypotension that are important during spinal needle projection, we also recorded hemodynamic responses that were not studied in previously mentioned studies.
There were statistical differences in MAP and HR at third minutes after the spinal puncture between the ball and the control groups, these differences were not related to valsalva maneuver.
In conclusion we suggest that Valsalva maneuver can decreases the skin puncture pain associated with spinal needle projection while observing hemodynamic changes.
Acknowledgements
This study was supported by a grant from Tehran University of medical Sciences.
Implications Statement: Valsalva maneuver can decrease the severity of spinal needle projection pain with no significant clinical hemodynamic changes.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Gajraj NM, Sharma S, Souter AJ, Pole Y, Sidawi E. A survey of patients who refuse regional anesthesia. Anesth Analg. 1994;78:s126
2. Morris RW, Whish DKM. A controlled trial of pain on skin infiltration with local anesthetics. Anesth and inten care. 1984;12:113-4
3. Morris R, McKay W, Mushlin P. Comparison of pain associated with intradermal and subcutaneous infiltration with various local anesthetic solutions. Anesth Analg. 1987:1180-2
4. Kocielniak-Nielsen Z, Hesselbjerg L, Brushoj J. et al. EMLA patch for spinal anesthesia, a comparison of EMLA patch with lidocaine infiltration and placebo patch. Anesthesia. 1998;53:1209-1227
5. Patterson P, Hussa AA, Fedele KA. et al. Comparison of 4 analgesic agents for venipuncture. AANA J. 2000;68:43-51
6. Usichenko TI, Pavlovic D, Foellner S, Wendt M. Reducing venipuncture pain by a cough trick: a randomized crossover volunteer study. Anesth Analg. 2004;98:343-5
7. Agarwal A, Sinha P.K, Tandon M, Dhiraaj S, Singh U. Evaluating the Efficacy of the Valsalva Maneuver on Venous Cannulation Pain: A Prospective, Randomized Study. Anesth Analg. 2005;101:1230-2
8. Gupta D, Agrawal A, Dhiraaj S. et al. An evaluation of balloon inflation on venous canulation pain in children: a prospective, randomized, controlled study. Anesth Analg. 2006;102:1372-5
9. Randich A, Maixner W. Interaction between cardiovascular and pain regulatory systems. Neurosci Biobehav Rev. 1984;8:343-67
10. Ghione S. Hypertension - associated hypalgesia. Evidence in experimental animal and humans, pathophysiological mechanisms, and potential clinical consequences. Hypertension. 1996;28:494-504
Author contact
![]() Corresponding author: Gita Shoeibi, M.D. Department of Anesthesiology, Dr Shariati Hospital, North Kargar Street, Ale-Ahmad Highway, Tehran 1411713135, IRAN. Tel: +98-912-1226683 (Cell); Fax: +98-21-88633039 (Hospital); E-mail: soltanmotums.ac.ir
Corresponding author: Gita Shoeibi, M.D. Department of Anesthesiology, Dr Shariati Hospital, North Kargar Street, Ale-Ahmad Highway, Tehran 1411713135, IRAN. Tel: +98-912-1226683 (Cell); Fax: +98-21-88633039 (Hospital); E-mail: soltanmotums.ac.ir

 Global reach, higher impact
Global reach, higher impact