Impact Factor
ISSN: 1449-1907
Int J Med Sci 2025; 22(10):2434-2445. doi:10.7150/ijms.114402 This issue Cite
Research Paper
The Immature Infant Liver: Cytochrome P450 Enzymes and their Relevance to Vaccine Safety and SIDS Research
1. Independent Researcher, P.O. Box 444, Bogue Chitto, MS 39629
2. Orthomolecular Medicine News Service, Cheng Integrative Health Center, 6149 St. Andrews Rd. Columbia, SC 29212
Received 2025-3-25; Accepted 2025-4-15; Published 2025-4-28
Abstract
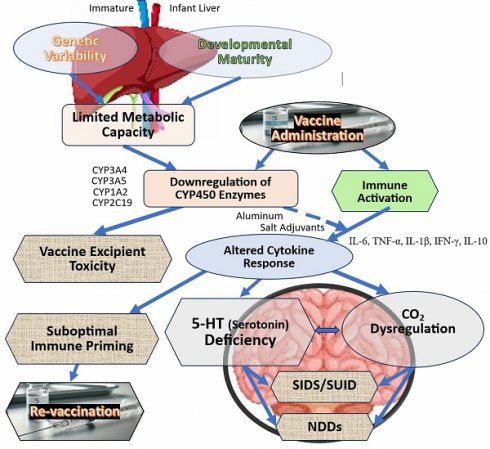
Aim and background: Vaccines are a cornerstone of modern medicine, significantly reducing morbidity and mortality worldwide. Their administration in infants requires consideration of physiological maturity. Cytochrome P450 (CYP450) enzymes, crucial for drug metabolism, are underdeveloped at birth and mature over the first two to three years of life. While vaccines are not directly metabolized by CYP450 enzymes, emerging evidence suggests that certain excipients—such as polysorbate 80 and gelatin—could interact with CYP450 pathways, particularly in genetically susceptible infants. This study integrates pharmacogenetics and epidemiology to examine how CYP450 immaturity and variability may influence vaccine excipient metabolism, immune activation, and infant health outcomes.
Methods: A systematic review of peer-reviewed literature, pharmacogenetic data, and epidemiological studies was conducted to assess CYP450 enzyme activity in infants, potential metabolic interactions with vaccine excipients, and temporal associations between vaccination and sudden infant death syndrome (SIDS). Gaps in postmortem investigations were also evaluated for their impact to identify metabolic vulnerabilities.
Results: CYP450 enzymes exhibit developmental immaturity in infants and genetic polymorphisms—particularly in CYP2D6 and CYP3A5—may affect vaccine excipient clearance. While epidemiological evidence shows temporal clustering of some SIDS cases post-vaccination, causality remains unproven. Inflammation-induced suppression of CYP450 enzymes raise questions about potential metabolic vulnerabilities, which current postmortem protocols often fail to capture.
Conclusion: This study highlights the need for further research into the influence of CYP450 variability on vaccine-related outcomes. Incorporating genetic and metabolic profiling into postmortem protocols may improve our understanding of metabolic contributions to SIDS and refine vaccine safety assessments.
Clinical significance: Developmental immaturity and genetic variability in CYP450 enzymes may affect vaccine excipient metabolism and interact with immune activation. This interplay could influence metabolic vulnerabilities in infants, particularly with inflammation-induced CYP450 suppression. Genetic and metabolic profiling before vaccination could identify at-risk infants, while postmortem analysis may enhance SIDS understanding and vaccine safety assessments.
Keywords: CYP450 enzymes, vaccine safety, infant vaccination, sudden unexpected infant death (SUID), sudden infant death syndrome (SIDS), Neurological Developmental Disorders (NDDs), cytochrome P450, pharmacogenetic screening
Introduction
Vaccines are a cornerstone of modern medicine, significantly reducing morbidity and mortality worldwide. Their administration in infants, however, requires consideration of physiological maturity. Cytochrome P450 (CYP450) enzymes, crucial for drug metabolism, are immature at birth and mature over time [1]. While these enzymes metabolize approximately 80% of clinical drugs [2, 3], the potential influence of CYP450 enzymes on the metabolism of vaccine excipients in infants remains under-investigated. This study examines how CYP450 enzyme immaturity and variability may influence the metabolism of vaccine excipients and its relevance to immune response and safety outcomes.
The CYP450 system includes 57 functional genes, with CYP1, CYP2, and CYP3 families metabolizing most clinical drugs [2, 3]. Genetic variations (i.e., polymorphisms), particularly in CYP2D6 and CYP3A5, contribute to interindividual variability in enzyme activity, which may affect how some infants process vaccine components [4]. While vaccines are not metabolized like traditional pharmaceuticals, certain excipients and adjuvants—such as aluminum salts and lipid nanoparticles—may interact with CYP450 pathways, influencing immune modulation in specific contexts [5,6]. Although the prevailing consensus is that vaccine excipients are present at trace levels and do not impact metabolism, the increasing complexity of vaccine formulations, including combining multiple novel adjuvants, underscores the need to investigate potential metabolic interactions in vulnerable populations.
Evidence from Johnson-Schmunk et al. [7] suggests that some vaccines may transiently suppress CYP3A4 activity, raising questions about potential interactions between vaccine components and metabolic processes. Additionally, adjuvants and excipients, including polysorbate 80 and gelatin, are known to interact with CYP450 enzymes—particularly CYP3A4—potentially affecting metabolism in individuals with specific polymorphisms [8]. In clinical practice, preterm infants with reduced CYP450 activity may exhibit altered immune responses, often requiring additional vaccine doses to achieve adequate immunity [9-11]. The possibility that cumulative exposure to vaccine excipients could lead to concentrations that exceed safe thresholds and impact CYP450 activity merits further investigation. While the established safety of vaccines is supported by extensive epidemiological evidence, the potential influence of CYP450 variability on vaccine metabolism and long-term outcomes warrants further investigation.
Although the precise etiology of sudden infant death syndrome (SIDS) remains unknown, neuropathological studies have consistently observed brainstem and medulla abnormalities in approximately 70% of SIDS cases [12]. Some emerging hypotheses suggest that reduced CYP450 function may contribute to prolonged exposure to inflammatory mediators, which could play a role in neurodevelopmental vulnerabilities, although direct evidence remains limited [13]. This connection, while speculative, highlights the need for further research into metabolic and inflammatory pathways in vulnerable populations.
In addition to the widely accepted hypothesis that attributes SIDS to brainstem dysfunction affecting cardiorespiratory regulation, an increasingly supported alternate hypothesis focuses on infection and inflammation as central contributors. This model highlights the role of inflammatory cytokines not merely as modulators of autonomic function, but as direct actors in the pathogenesis of SIDS. Autopsy studies have demonstrated convincing evidence in support of this, including increased organ weights (especially hepatic enlargement), widespread microglial and astroglial activation, and a notable association with recent viral infections. These findings underscore a broader inflammatory milieu that may operate independently of or in conjunction with brainstem-mediated mechanisms.
This study integrates pharmacogenetics and epidemiology to examine how CYP450 variability may influence vaccine metabolism, immune activation, and infant health outcomes. By addressing this underexplored area, we aim to contribute to a more comprehensive understanding of the factors shaping vaccine responses, particularly in metabolically immature and vulnerable pediatric populations. While this paper does not deny the public health benefits of vaccines, it raises important questions regarding how the genetic variability and the immaturity of CYP450 enzymes may influence vaccine-related outcomes in vulnerable populations.
Materials and Methods
Study focus
This study explores the implications of infant liver immaturity, specifically CYP450 enzyme development, on vaccine metabolism and infant health outcomes, including sudden infant death syndrome (SIDS). By integrating pharmacogenetics, epidemiology, and clinical research, the study examines how CYP450 variability may affect vaccine metabolism, immune responses, and safety in infancy.
Data sources and selection
This narrative review synthesizes peer-reviewed literature, pharmacogenetic studies, and epidemiological research on (1) CYP450 enzyme maturation in infants, (2) metabolism of vaccine excipients and adjuvants, (3) associations between vaccination and SIDS, and (4) postmortem findings of metabolic abnormalities in SIDS cases. No new experimental data were generated; existing research was critically analyzed to identify gaps in understanding infant vaccine metabolism.
Infant liver function and CYP450 enzymes
The study reviews CYP1, CYP2, and CYP3 enzyme maturation in infants, with a focus on how genetic polymorphisms (e.g., CYP2D6, CYP3A5) influence metabolic capacity and variability in vaccine component clearance. Preterm infants, with reduced CYP450 activity, are a key focus due to their altered vaccine metabolism.
Vaccine component metabolism
The study examines how vaccine excipients, including aluminum adjuvants and polysorbate 80, are metabolized by CYP450 enzymes in infants. It also looks at how polymorphisms in CYP2C and CYP2D6 may influence immune responses and risks for preterm infants, including respiratory issues and apnea.
Gaps in current research
Although CYP450 variability is well-established in drug metabolism, its role in vaccine metabolism remains underexplored. Direct measurements of CYP450 activity post-vaccination in infants are lacking, and current safety assessments often ignore genetic and developmental differences. This study identifies these gaps and calls for further research on pharmacogenetic factors in vaccine metabolism and safety.
Epidemiological and postmortem analysis
The study reviews epidemiological studies on vaccination and SIDS, alongside postmortem reports of metabolic abnormalities. It emphasizes the need for refined postmortem protocols to assess metabolic factors, such as CYP450 activity, in vaccine-related infant mortality.
This narrative study aims to instill motivation toward the important goal of advancing our understanding of metabolic factors influencing vaccine responses, thereby encouraging further research in pediatric pharmacogenetics and vaccine safety.
Background
Potential involvement of CYP450 enzymes following vaccination
Infant CYP450 enzyme expression is incomplete at birth, with significant developmental variability. This immaturity reduces the ability to metabolize substances, including vaccine excipients, and may be compounded by genetic polymorphisms. CYP450 enzyme activity is typically at 30-60% of adult levels at birth [14], with maturation occurring gradually over the first few years of life [15]. Polymorphisms in CYP2D6 or CYP3A5, can modulate enzyme activity during this period, potentially influencing how vaccine excipients are metabolized. Additionally, developmental immaturity can reduce capacity during this period, influencing how vaccine excipients are metabolized [16].
Vulnerable infants and immune response variability
Vulnerable infants, particularly preterm ones, exhibit variability in immune responses to vaccines. Preterm infants may not reach protective antibody levels due to underdeveloped immune and metabolic systems, linked to a diminished cytokine response [14,17]. CYP450 polymorphisms may affect the metabolism of vaccine excipients, thereby influencing immune activation. While genetic variations remain constant, enzyme activity evolves during early development, affecting how vaccine excipients are processed [18].
Influence of genetic polymorphisms on enzyme function
Inherited CYP450 polymorphisms influence enzyme function, leading to metabolic phenotypes ranging from poor to ultrarapid metabolizers. For example, individuals with the CYP2D6*4 variant (a specific genetic change in the CYP2D6 gene) exhibit reduced enzyme activity, while those with CYP2D6*2 or CYP2C19*17 may metabolize substances more rapidly, potentially affecting immune response timing and strength [14,15,17,19].
Metabolizer status in preterm vs. term infants
Table 1 shows the prevalence of metabolizer types in preterm and term infants. Preterm infants are more likely to exhibit poor or intermediate metabolic activity due to immature enzyme systems. Certain term infants generally have a broader range of normal to ultrarapid metabolism. Some preterm infants of African descent, may express functional CYP3A5, influencing their metabolizer status [13,17,20].
Cumulative exposure to vaccine excipients
Although vaccine excipients are present at reduced or trace levels per dose, cumulative exposure from multiple vaccines administered in early infancy could exceed safe thresholds in infants with CYP450 polymorphisms [15]. While direct studies on vaccine excipients and CYP450 metabolism are limited, research on chemically similar compounds suggests potential enzyme interactions [19]. The immaturity of metabolic pathways during infancy may reduce the capacity to detoxify or eliminate vaccine excipients, raising concerns about cumulative impacts [14, 15, 19].
Need for further research
Further research is needed on the metabolic handling of vaccine excipients and the potential influence of CYP450 enzyme polymorphisms on excipient metabolism and safety [14,15]. Investigating these pharmacokinetic variables may clarify whether specific excipients, when administered in multiple doses, affect CYP450 activity and metabolic homeostasis in infants [19].
Vaccines and their excipients
Vaccines contain active components (antigens) that stimulate the immune response, and inactive components (excipients) that enhance the vaccine's stability and safety. Excipients include adjuvants such as aluminum salts that enhance immune responses but may be metabolized differently based on CYP450 enzyme activity [21,22]. Adjuvants stimulate immune activation, including the release of cytokines, which modulate and regulate the immune response [23]. In infants, with immature enzyme systems, polymorphisms in genes such as CYP2D6 or CYP3A5 could affect excipient metabolism, potentially altering vaccine efficacy and safety [24]. Preservatives and stabilizers may also influence the overall immune responses [25].
Genetic variations in CYP450 enzymes result in differences in how quickly or slowly vaccine excipients are cleared impacting vaccine safety and efficacy, particularly in vulnerable infant populations [26]. Understanding these metabolic differences is crucial, as CYP450 enzyme activity is immature at birth, complicating predictions in relevant infants, whose CYP450 enzyme activity is often immature at birth, further complicating the prediction of immune responses [14].
Table 2 provides a list of key vaccine excipients and their respective roles or mechanisms in vaccine formulations. Additionally, for a child under the age of two years, Table 3 details each recommended vaccine, number of doses, administration time, and key excipients.
Excipients and CYP450 interactions
While the cytochrome P450 (CYP450) enzyme system is generally not responsible for metabolizing or detoxifying many of the key vaccine excipients (Table 3), some may interact with specific CYP450 enzymes [8]. Table 4 identifies excipients that could impact CYP450 activity in infants and fetuses [21,22]. Although excipients are formulated to be safe per dose, repeated exposure could lead to cumulative concentrations exceeding safe thresholds, potentially impacting CYP450 activity [27].
Generalized CYP450 enzymes: their preterm and term prevalence with respect to each metabolizer type.
| Metabolizer type | Preterm infants (%) | Term infants (%) |
|---|---|---|
| Poor (PM) | 15 to 401 | 5 to 15 |
| Intermediate (IM) | 30 to 50 | 10 to 30 |
| Normal or Extensive (EM) | 20 to 40 | 50 to 80 |
| Ultrarapid (UM) | Variable, generally <52 | 1 to 103 |
1Higher prevalence in certain enzymes such as CYP1A2 and CYP2C19.
2CYP3A5 expression in preterm infants varies by ethnicity: 10-30% in African descent, 3-7% in Asians, <1% in Europeans, 3-10% in Latinos, and 5-15% in Middle Easterners.
3In term infants, CYP3A5 ultrarapid metabolizer prevalence is higher in certain populations: 40-70% in African descent, <5% in Europeans, 10-20% in Asians and Latinos, and 20-30% in Middle Easterners.
Key vaccine excipients and their roles.
| Excipient | Role |
|---|---|
| Adjuvant | Enhances immune response by stimulating the Th2 response. |
| Preservative | Prevents microbial contamination in multi-dose vials. |
| Stabilizer | Maintains vaccine effectiveness during storage and transport. |
| Inactivating agent | Kills or inactivates pathogens while preserving immunogenicity. |
| Buffer | Maintains pH stability to prevent degradation of active ingredients. |
| Residual | Trace substances from manufacturing (e.g., antibiotics, and cell media). |
| Emulsifier | Stabilizes and disperses vaccine components |
| Antibiotic | Prevents bacterial contamination during manufacturing. |
Beyond direct interactions, immune activation post-vaccination influences CYP450 expression. Pro-inflammatory cytokines downregulate enzymes like CYP3A4, CYP2C19, and CYP1A2 [5,7,32], affecting drug metabolism and bioavailability. Given infants' immature metabolic pathways, repeated exposures could have cumulative effects [14,17].
CYP450 system and aluminum exposure
The CYP450 system plays a critical role in metabolic detoxification, including substances such as aluminum salts, which are widely used as vaccine adjuvants. While regulatory bodies maintain that aluminum exposure remains within safe limits, concerns persist regarding neurotoxicity in developing infants [27]. Unlike oral aluminum, which has low bioavailability, intramuscular aluminum is nearly 100% bioavailable (albeit released from the muscle over time) increasing the risk of exceeding safe thresholds and impairing renal and hepatic function [27]. Given its cumulative nature, aluminum's potential to disrupt CYP450-mediated metabolism warrants further evaluation.
Immune system activation on CYP450 enzymes
Cytokine-mediated CYP450 suppression may alter drug metabolism, impacting co-administered medications' efficacy and safety [16,28,29]. The cumulative effect of vaccine excipients and immune responses on CYP450 activity requires further study to assess long-term effects [15,18,28].
Vaccine doses, administration time (months), and key excipients in pediatric immunization (under 2 years).
| Vaccine (abbr.) | Total doses | Age (months) of dose admin. | Key excipients1 (role code) |
|---|---|---|---|
| Hepatitis B (HepB) | 3 | Birth, 1-2, 6-18 | Aluminum hydroxide (A), Sodium chloride (S), Sodium dihydrogen phosphate dihydrate (B), Disodium phosphate dihydrate (B), Yeast protein (R), Formaldehyde (I) |
| Rotavirus (RV) | 2 or 3 | 2, 4, 6 | Sodium citrate (B), Sodium phosphate monobasic monohydrate (B), Sucrose (S), Polysorbate 80 (E & S}, Sodium hydroxide (B), Fetal bovine serum (R) |
| Diphtheria, Tetanus, and acellular Pertussis (DTaP) | 4 | 2, 4, 6, 15-18 | Aluminum phosphate (A), Formaldehyde (I), Glutaraldehyde (I), 2-Phenoxyethanol (P), Polysorbate 80 (E & S), Sucrose (S), Sodium chloride, Neomycin sulfate (T & R), Polymyxin B sulfate (R) |
| Haemophilus influenzae type b (Hib) | 3 or 4 | 2, 4, 6, 12-16 | Aluminum phosphate (A), Monophosphoryl Lipid A—MPLA (A), Formaldehyde (i), Polysorbate 80 (E & S), Sucrose (S), Lactose (S), Sodium chloride (B), Sodium phosphate (B) |
| Pneumococcal Conjugate (PCV15 or PCV20) | 4 | 2, 4, 6, 12-15 | Aluminum phosphate (A), Phenol (P), Polysorbate 80 (E & S), Sucrose (S), Sodium chloride (B), Dipotassium phosphate (B), Sodium phosphate (B), Succinic acid (B) |
| Inactivated Poliovirus2 (IPV) | 3 | 2, 4, 6-18 | Formaldehyde (I), 2-Phenoxyethanol (P), Polysorbate 80 (E & S), Neomycin sulfate (T & R), Polymyxin B sulfate (T & R), Sodium chloride (B), Dipotassium phosphate (B), Sodium phosphate (B), Sucrose (S) |
| Inactivated Influenza2 (inactivated) (IIV) | 3 | 6, 7-8, annual dose starting at 12 months | Aluminum hydroxide (A), Formaldehyde (I), Sodium chloride (B), Sucrose (S), Polysorbate 80 (E & S), Gentamicin sulfate (T & R), Neomycin sulfate (T & R), Kanamycin sulfate (T & R), Polymyxin B (T & R), Egg protein (R) |
| Measles, Mumps, and Rubella (MMR) | 1 | 12-15 | Neomycin sulfate (T & R), Gelatin (S), MSG (S), Sorbitol (S), Sodium chloride (B), Sodium phosphate (B), Chlorpyrifos (R), Diphosphates (B), Sucrose (S), Human serum albumin (S), Recombinant human albumin (S), Amino acids (S & B), Fetal bovine serum (S & R) |
| Varicella (VAR) | 1 | 12-15 | Neomycin sulfate (T & R), Gelatin (S), Sucrose (S), MSG (S), Sodium Phosphate (B), Polysorbate 80 (E & S), Neomycin sulfate (T & R) |
| Hepatitis A (HepA) | 1 | 12-23 | Aluminum hydroxide (A), Formaldehyde (I & R), Polysorbate 20 or 80 (E & S), MSG (S), Sodium phosphate dibasic (B), Monosodium phosphate (B), Neomycin sulfate (T & R) |
| COVID-19 (mRNA) | 3 | 6, 7-8, 10 | Lipid nanoparticles: LNPs with Polyethylene Glycol (S & E), Potassium chloride (B), Potassium phosphate (B), Sodium chloride (B), Sodium phosphate (B), Sucrose (S) |
1Excipient role codes: A-adjuvant, B-buffer, E-emulsifier, I-inactivating agent, P-preservative, R-residual, S-stabilizer, T-antibiotic. Specific excipients can vary by vaccine manufacturer and formulation.
2IIV (Inactivated Influenza Vaccine) Egg-based: residual antibiotics and egg proteins; cell-based: antibiotic-free and has no egg proteins.
Vaccine excipients potentially impacting CYP450 enzymes in infants (<12 months) and fetuses.
| Vaccine(s) | Excipients1 that potentially impact CYP450 enzymes | CYP450 enzyme(s) involved | Metabolic role |
|---|---|---|---|
| DTaP, HepB, Hib, PCV | Aluminum hydroxide/phosphate2 | CYP1A2, CYP2D6, CYP3A4, CYP2C9 | Cytokine-mediated CYP450 downregulation. |
| Rotavirus, MMR, Varicella | Live attenuated rotavirus | CYP1A2, CYP2D6, CYP3A4, CYP2C9 | Immune activation leading to cytokine-mediated CYP450 downregulation. |
| COVID-19 Vaccine | Lipid nanoparticles (LNPs) | CYP2C19, YP3A4, CYP2E1 | LNP-induced cytokine release may suppress CYP450 modulation. |
| Hepatitis B (pregnancy) | Aluminum hydroxide/phophate2 | CYP1A2, CYP2D6, CYP3A4, CYP2C9 | Indirect immune modulation. |
| COVID-19 (pregnancy) | Lipid nanoparticles (LNPs) | CYP2C19, CYP3A4, CYP2E1 | Immune modulation and potential metabolic effects. |
1Excipients not included in this table: Polysorbate 80 and/or Formaldehyde found in trace amounts in DTaP, HepB, PCV (Pneumococcal conjugate vaccine), RV (Rotavirus Vaccine), and vaccines given during pregnancy—TdaP, Inactivated Influenza (IIV), and COVID-19.
2Refer to CYP450 interactions described below in the “Reevaluating Infant aluminum exposure” section.
Reevaluating infant aluminum exposure
Aluminum-based adjuvants such as aluminum hydroxide (Al(OH)₃) and aluminum phosphate (AlPO₄) are routinely used in infant vaccines such as HepB, DTaP, PCV, and Hib, with infants receiving approximately 3,350 mcg of aluminum within the first year. The FDA's 2011 safety assessment uses a 0.78% bioavailability estimate [28], whereas the ATSDR's estimate of 0.1% estimate [27] suggests the FDA's risk assessment may be overestimated by a factor of 7.8 (0.78%/0.1%=7.8) [29].
Though aluminum is primarily cleared by the kidneys, its prolonged retention at the injection site, along with immune activation, may indirectly influence CYP450 enzymes in the liver. CYP450 enzymes are involved in the metabolism of drugs, hormones, and toxins. Aluminum-induced immune responses can lead to cytokine release, which has been shown to downregulate certain CYP450 enzymes like CYP3A4 and CYP2C19. This downregulation could impair the liver's ability to metabolize medications or other substances effectively, potentially altering their bioavailability and efficacy. Given infants' immature renal and metabolic functions, the cumulative exposure to aluminum from multiple vaccines could impact CYP450 activity, with implications for both drug interactions and metabolic health [14,17].
Formaldehyde and polysorbate 80: the need for further research
Formaldehyde and Polysorbate 80 (Tween 80) function as stabilizers and adjuvants in vaccines but may transiently elevate systemic levels upon intramuscular administration. Vaccine formulations contain formaldehyde in varying amounts (e.g., DTaP: 100 µg/dose, HepB: <30 µg/dose, IPV: 7.5-15 µg per dose), while Polysorbate 80 is present in select vaccines. Although these compounds are generally regarded as safe, their intramuscular pharmacokinetics remain underexplored, particularly regarding CYP450 interactions [14,15].
Formaldehyde is rapidly converted to formate, yet transient spikes may occur post-administration. Polysorbate 80 has been implicated in blood-brain barrier permeability and could interact with other excipients. While neither compound accumulates in tissues, their cumulative metabolic effects, particularly in infants with developing enzymatic systems, require further investigation [6,20].
The long-term implications of repeated exposure to these excipients, especially in combination with other vaccine components, remain uncertain and warrant continued toxicological and pharmacokinetic research [30]. Although neither formaldehyde nor Polysorbate 80 accumulates in tissues like the brain or bones (unlike aluminum), the long-term effects remain unclear. Continued pharmacokinetic and toxicological research is needed to assess their impact on CYP450 enzymes, metabolic pathways, neurodevelopment, and long-term safety for developing children [8,18].
Results
Studies implicating CYP450 involvement in SIDS
Research from Treluyer et al. [31] and Prandota [32] suggests that (1) CYP2C enzyme expression in infants may contribute to apnea, increasing vulnerability to SIDS, and (2) cytokine-induced inflammation following vaccination may prolong exposure to vaccine components or cytokine-inducing adjuvants due to metabolic insufficiency, especially in infants with immature enzyme systems. This supports our hypothesis that reduced CYP450 enzyme activity, potentially exacerbated by genetic variations, could impact vaccine metabolism and increase the risk of respiratory events such as SIDS.
Almost 40 years ago, Hunt and Brouillette [33] noted that abnormal neuro-regulation of cardiorespiratory control in the brainstem remains a compelling hypothesis in SIDS research, a theory that has gained renewed relevance in light of recent independent brainstem pathology reports in SIDS cases [32].
Kinney et al. [34] report that the most consistent neurochemical abnormality in SIDS cases, and most likely to be pathophysiologically significant [35], involves the medullary 5-HT (serotonin) system, implicated in approximately 70% of cases. This abnormality has been confirmed across multiple independent datasets and laboratories [35-38]. Dysfunction in this system may impair an infant's arousal response to rising carbon dioxide levels, increasing the risk of fatal apnea episodes. As Kashiwagi et al. [39] state, “All effective vaccines induce the production of cytokines or chemokines, which modulate immunogenicity.”
Given that cytokine-induced inflammation can suppress CYP450 enzyme activity, as shown in studies by Deb and Arrighi [13], it is plausible that reduced CYP function prolongs exposure to inflammatory mediators. This could, in turn, exacerbate disruptions in the 5-HT system, potentially impairing respiratory and autonomic regulation in vulnerable infants. Thus, the interplay between vaccine-induced cytokine responses, CYP450 enzyme activity, and serotonin-mediated arousal mechanisms forms the basis of our hypothesis, warranting further investigation in the context of SIDS.
Vaccine-induced apnea in preterm infants
The randomized controlled trial by Greenberg et al. [40] investigated the effects of two-month vaccinations in hospitalized preterm infants (<33 weeks gestation). Among the 223 infants studied, those who received vaccinations exhibited higher odds of apnea within 48 hours compared to unvaccinated controls. While the frequency and severity of apneic events were comparable between groups, the increased occurrence of apnea episodes suggests a potential interaction between immune activation and respiratory control in preterm infants.
Since CYP450 enzyme activity is still developing in this population—particularly the transition from fetal CYP3A7 dominance [15] to postnatal CYP3A4 function—metabolic insufficiency could lead to prolonged inflammatory responses or delayed clearance of vaccine components. This supports our hypothesis that some preterm infants, particularly those with CYP polymorphisms, may be more vulnerable to immune-mediated respiratory effects following vaccination. However, no serious adverse events were observed during the 48-hour monitoring period, likely due to timely intervention in response to the use of respiratory and pulse oximetry alarms in hospitalized preterm settings.
Potential association between vaccination and SIDS
A review of epidemiological studies indicates that SIDS and sudden unexpected infant death (SUID) cases peak within the same age range as routine infant vaccinations, prompting investigation into a possible connection. Miller [41] considered the relationship between vaccines and sudden infant death, presenting results from his own study and identifying six additional independent studies that failed to report a uniform distribution of SIDS cases following vaccine administration, as would be expected if the pattern were coincidental. Miller's analysis of 2,605 cases of infant death reported from 1990 to 2019 from the Vaccine Adverse Event Reporting System (VAERS) database revealed a significant non-random distribution of SIDS reports following vaccination—approximately 75% of reports occurred within the first week, with a peak on day two, and the remaining 25% occurred between 8 and 60 days (p<.00001) [41]. Although this correlation is not evidence of causation, it highlights the need for further controlled studies to determine whether the association is due to a direct vaccine effect or other coinciding factors.
Misclassification of SIDS cases in postmortem investigations
Evidence from autopsy reviews and legal case testimony suggests that current SIDS investigations might not capture all relevant neuropathological findings. For example, the Boatmon v. Secretary of Health and Human Services case recognized that neuropathological examinations were not consistently performed [42].
Ottaviani et al. [43] have argued that limited autopsy protocols could contribute to underreporting deaths temporally associated with vaccination. Additionally, Kuhnert et al. [44] documented a 16-fold increase in sudden deaths following pentavalent or hexavalent vaccines, and Zinka et al. [45] described six cases of post-vaccine SIDS with abnormal brain findings that may suggest—but do not conclusively prove—a potential association.
Genetic variability in CYP450 and vaccine metabolism
Analysis of pharmacogenetic data indicates that CYP450 polymorphisms can influence the metabolic response to vaccine excipients. Infants are classified into four metabolic phenotypes (poor, intermediate, extensive, ultrarapid metabolizers)—each reflecting individual differences in detoxification capacity [4,46,47]. Preliminary evidence suggests that infants classified as poor metabolizers may experience prolonged exposure to vaccine components, potentially increasing the risk of adverse reactions. However, further research is needed to clarify the clinical significance of these findings.
Beyond genetic polymorphisms, developmental changes in metabolic enzyme expression further shape an infant's ability to process vaccine components. CYP3A7, the predominant enzyme in the fetal liver, facilitates drug and toxin metabolism before birth. However, its activity declines postnatally as CYP3A4 gradually replaces it. This transition period creates a metabolic bottleneck, particularly in preterm infants who still rely on CYP3A7 for clearance. This reduced capacity of the CYP450 system to perform its functions during this transition could lead to delayed detoxification of vaccine-related substances, prolonging systemic exposure and increasing the risk of adverse events. Understanding how this enzymatic shift influences vaccine metabolism is crucial for refining individualized safety assessments and guiding future pharmacogenetic research.
Potential role of pharmacogenetic testing in clinical practice
Despite increasing evidence of the role of CYP450 in neonatal metabolism, pharmacogenetic testing remains uncommon in routine clinical practice. Barriers include limited clinician awareness, the absence of standardized clinical guidelines, and the inherent complexity of CYP450 interactions [48]. Nonetheless, targeted genetic screening for variants in genes such as CYP2D6, CYP3A5, and CYP1A2 may provide an individualized risk assessment before vaccination. This could, in theory, improve safety outcomes for certain high-risk infants, though further validation is required.
Discussion
Variability in SIDS/SUID postmortem protocols
Inconsistencies in postmortem protocols of SIDS/SUID
SIDS and sudden unexpected infant death (SUID) remain leading causes of post-neonatal mortality, yet inconsistencies in postmortem protocols may obscure contributing factors. Current classification methods rely heavily on autopsy findings, but variability in diagnostic criteria and forensic procedures can lead to misclassification. Comprehensive neuropathological examinations have, in some cases, identified congenital brainstem abnormalities, cardiac arrhythmias, or metabolic disorders that standard autopsies may overlook. Standardizing forensic investigations could enhance the accuracy of SIDS classification and reduce potential misdiagnoses.
A key challenge in investigating SIDS/SUID
The Boatmon case underscores a fundamental limitation in SIDS research—neuropathological examinations often lack sufficient tissue sampling, missing critical brain regions such as the medulla and hippocampus [42]. Studies by Ottaviani et al. [43] and Zinka et al. [45] suggest that enhanced postmortem protocols could reveal underlying neuropathological findings in cases otherwise labeled as unexplained SIDS. Implementing standardized protocols across jurisdictions could provide greater clarity regarding SIDS pathology and potential contributing factors.
CYP450 enzymes and their potential role in SIDS
Indirect link between CYP450, apnea, and cytokine-induced inflammation
A growing body of research suggests that cytokine-induced inflammation can transiently suppress CYP450 enzyme activity, potentially prolonging respiratory vulnerability in metabolically susceptible infants. While prior studies have linked inflammatory cytokines to apnea, our findings indicate that compromised CYP450 function may extend this effect, creating an increased period of respiratory risk. These results highlight the need for further research into whether CYP450 polymorphisms may heighten susceptibility to vaccine-related cytokine responses.
Potential role of CYP450 immaturity in SIDS and neurodevelopmental outcomes
While serotonin dysregulation remains a predominant focus in SIDS research, emerging evidence suggests that CYP450 enzyme immaturity may serve as a common denominator linking SIDS, neurodevelopmental disorders (NDDs), and other infant health conditions. Underdeveloped CYP450 enzyme systems not only contribute to respiratory vulnerability but could also have long-term implications for neurodevelopment. Limited metabolic capacity in early life increases susceptibility to toxic exposures, potentially influencing conditions such as autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), epilepsy, and learning disabilities. Polymorphisms in CYP3A4, CYP2C19, and CYP1A2 could impair detoxification of environmental toxicants, while dysfunction in CYP2E1 and CYP2D6 has been linked to oxidative stress and mitochondrial impairment—both implicated in neurodevelopmental delays.
Temporal patterns and case studies of post vaccine SIDS
SIDS reports are clustered, not uniformly distributed following vaccination
VAERS data indicate a temporal clustering of SIDS cases within the first week post-vaccination, peaking on day two [41]. This is an important observation—if these cases were simply coincidental, we would expect a more uniform daily distribution of reports. However, the specific peak on day two and clustering within the first week post-vaccination raises the question of whether immune activation or other transient physiological effects could contribute to this timing. Miller [41] details six other studies that show similar clustering in the first week using different methodologies and populations, which warrants further investigation to determine if this clustering reflects an unrecognized biological mechanism or is attributable to confounding factors.
Another important consideration is the real-world context in which vaccines are administered. Infants often receive vaccinations in busy clinics or doctors' offices, where the potential for exposure to circulating pathogens is elevated. This raises the possibility that simultaneous exposure to both vaccine-induced immune stimulation and a coincidental or subclinical infection could result in a heightened inflammatory state. Such a scenario may lead to an additive or even synergistic increase in proinflammatory cytokine levels—essentially, “inflammatory cytokines on top of inflammatory cytokines.” This layered immune activation could be particularly significant in infants with immature or genetically predisposed metabolic systems, and may help explain why some adverse outcomes, though rare, appear to cluster temporally following vaccination.
SIDS in a four-month-old following receipt of five vaccines
In Boatmon v. Secretary of Health & Human Services [42], a four-month-old infant, previously healthy, received five vaccines (DTaP, IPV, PCV, RV, and HepB) during a well-baby visit. The following day, he developed a fever and later died unexpectedly. Despite an autopsy classifying the case as SIDS, neuropathologist Dr. Douglas C. Miller presented literature suggesting that vaccine-induced inflammatory cytokines could act as potential triggers in susceptible infants. While the original ruling recognized a “medically acceptable temporal relationship,” the decision was later reversed upon appeal, highlighting the broader challenge of establishing causality between vaccination and SIDS in legal and scientific contexts.
Some deaths misclassified as SIDS obscure vaccine-related outcomes
Recent studies (Kuhnert et al. [44], Zinka et al. [45]) emphasize the need for systematic reassessment of unexplained post-vaccination deaths. Additionally, Ganjare et al. [49] highlight the role of neurotransmitter and metabolic imbalances in SIDS cases. If CYP450 enzyme immaturity contributes to metabolic vulnerabilities, it is possible that some cases currently classified as SIDS involve undetected biochemical contributors. This underscores the importance of refining postmortem analyses to account for potential metabolic influences.
While individual vaccine components are considered safe at standard doses, cumulative exposure across the first year of life—where infants receive 24 to 26 vaccine doses—raises significant concerns about metabolic capacity in genetically susceptible populations. This warrants further investigation, especially in light of studies showing that early-life metabolic vulnerabilities could be exacerbated by multiple vaccine doses.
Greenberg et al. [40] evaluated the short-term safety of vaccinating preterm infants at two months' chronological age and found no severe adverse events within 48 hours, supporting current vaccination guidelines for hospitalized preterm infants. However, these findings do not address potential long-term neurodevelopmental consequences, an area requiring further study.
A retrospective analysis [50] of 47,155 Florida Medicaid records (1999-2011) identified a statistically significant association between vaccination and increased odds of NDDs. By age nine, vaccinated children had increased odds of ASD (OR 2.7) and tic disorder (OR 6.2) compared to unvaccinated peers. Among 5,009 preterm children (89.7% vaccinated), vaccinated preterms exhibited significantly elevated odds of ASD (OR 3.14, 95% CI: 1.54-6.39), hyperkinetic syndrome (OR 3.0, 95% CI: 2.25-3.99), epilepsy/seizures (OR 4.17, 95% CI: 2.77-6.28), learning disorders (OR 9.84, 95% CI: 3.14-30.84), and encephalopathy (OR 7.12, 95% CI: 2.93-17.31) relative to unvaccinated preterms, with tic disorders absent among the unvaccinated group. While all epidemiological studies have limitations, Mawson's study is notable for its unique methodology, allowing for a direct comparison of long-term health outcomes in vaccinated and unvaccinated children. Although Mawson's study does not directly address vaccine excipients, the findings indirectly support concerns regarding early vaccination and its long-term impact on neurodevelopment.
Future directions in personalized medicine and research
The investigation into CYP450 enzyme variability underscores the importance of personalized medicine, particularly in vulnerable populations such as preterm infants. As research advances, a greater emphasis on understanding genetic polymorphisms and their influence on drug metabolism could guide more precise therapeutic interventions [51]. Comprehensive pharmacokinetic studies focusing on age-specific enzyme activity could offer valuable insights into individual metabolic capacities [52]. Emerging technologies, including advanced metabolomics, hold promise for elucidating complex metabolic interactions and their implications for infant health. These approaches could refine our understanding of how CYP450 enzyme variability influences both short-term vaccine responses and long-term neurodevelopmental outcomes, fostering tailored medical approaches that prioritize safety and efficacy [53]. As a suggestion for future research, it may also be worth exploring whether any interaction exists between routine infant vaccinations and susceptibility to COVID-19 infection, although current evidence suggests such outcomes were rare.
Clinical significance
Recognizing the variability in CYP450 enzyme activity has significant clinical implications for neonatal and pediatric care. Improved screening for genetic polymorphisms related to CYP450 enzymes could enhance risk stratification and therapeutic decision-making. For instance, identifying infants with poor or ultrarapid metabolizer phenotypes could help clinicians optimize drug dosages, minimizing adverse effects while ensuring therapeutic efficacy. Additionally, understanding the metabolic impact of vaccine excipients and cumulative exposures could inform safer immunization practices. Integrating these insights into clinical practice may ultimately improve patient outcomes by aligning therapeutic interventions with individual metabolic profiles.
Conclusions
While vaccines are widely regarded as safe and effective, emerging evidence suggests that CYP450 enzyme immaturity, cytokine response, and metabolism may contribute to adverse reactions in genetically predisposed infants. Current vaccination schedules, which do not fully account for individual variability in metabolism, overlook the impact of polymorphisms in enzymes like CYP2D6, CYP2C19, and CYP3A4. This may lead to prolonged exposure to potentially toxic excipients or altered immune responses in infants with poor metabolizer phenotypes.
Pharmacogenetic screening could offer a more personalized approach to immunization, refining risk-benefit assessments before vaccine administration. Large-scale genetic studies and prospective research are needed to evaluate the safety and public health implications of this approach. Given the complex relationship between metabolic factors, vaccine responses, and conditions such as SIDS and neurodevelopmental disorders, further research into personalized immunization protocols may improve vaccine safety and clinical outcomes.
Integrating pharmacogenomics into vaccine risk assessment could pave the way for a precision-based immunization strategy, ensuring both safety and efficacy for all infants.
Abbreviations
5-HT: hydroxytryptamine (chemical name for serotonin); ADHD: Attention-Deficit/Hyperactivity Disorder; ASD: Autism Spectrum Disorder; CI: confidence interval; CYP450: Cytochrome P450; DTaP: Diphtheria, Tetanus, and acellular Pertussis vaccine; EM: extensive (or normal) metabolizer; HepA: Hepatitis A vaccine; HepB: Hepatitis B vaccine; Hib: Haemophilus influenzae type b vaccine; IIV: Inactivated Influenza vaccine; IM: intermediate metabolizer; IPV: Inactivated Polio vaccine; LNPs: lipid nanoparticles; MMR: Measles, Mumps, and Rubella vaccine; MPLA: Monophosphoryl Lipid A; mRNA: messenger RNA; NDD: Neurodevelopmental Disorder; OR: odds ratio; PCV: Pneumococcal Conjugate vaccine; PM: poor metabolizer; RV: Rotavirus vaccine; SIDS: sudden infant death syndrome; SUID: sudden unexpected infant death; UM: ultrarapid metabolizer; VAERS: Vaccine Adverse Event Reporting System; VAR: Varicella vaccine.
Author contributions
Conceptualization, GG; methodology, GG and RC; formal analysis, GG and RC; investigation, GG and RC; writing—original draft preparation: GG and RC; writing—review and editing: GG. All authors have read and agreed to the published version of the manuscript.
Competing interests
GSG is an editor and contributor to Orthomolecular Medicine News Service (OMNS). RZC is Editor-in-chief of OMNS, publishing free, online peer-reviewed content. GSG is an unpaid consultant for the non-profit Physicians for Informed Consent.
References
1. Sadler NC, Nandhikonda P, Webb-Robertson BJ. et al. Hepatic Cytochrome P450 Activity, Abundance, and Expression Throughout Human Development. Drug Metab Dispos. 2016;44:984-991
2. Sim SC, Ingelman-Sundberg M. The Human Cytochrome P450 (CYP) Allele Nomenclature website: A peer-reviewed database of CYP variants and their associated effects. Hum Genomics. 2010;4:278-281
3. Wang X, Ro J, Tan Z, Xun T, Zhao J, Yang X. Inflammatory signaling on cytochrome P450-mediated drug metabolism in hepatocytes. Front Pharmacol. 2022;13:1043836
4. Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism; regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138:103-141
5. Morgan ET. Impact of infectious and inflammatory disease on cytochrome P450-mediated drug metabolism and pharmacokinetics. Clin Pharmacol Ther. 2009;85:434-438
6. Dresser GK, Spence JD, Bailey DG. Pharmacokinetic-pharmacodynamic consequences and clinical relevance of cytochrome P450 3A4 inhibition. Clin Pharmacokinet. 2000;38:41-57
7. Johnson-Schmunk K, Ghose R, Croyle MA. Immunization and drug metabolizing enzymes: focus on Hepatic cytochrome P450 3A. Expert Rev Vaccines. 2021;20:623-634
8. Pellegrino P, Perrotta C, Clementi E, Radice S. Vaccine-Drug Interactions: Cytokines, Cytochromes, and Molecular Mechanisms. Drug Saf. 2015;38:781-787
9. Fan W, Zhang M, Zhu Y, Zheng Y. Immunogenicity of hepatitis B vaccine in preterm or low birth weight infants: A meta-analysis. Am J Prev Med. 2020;59:278-287
10. Golebiowska M, Kardas-Sobantka D, Chlebna-Sokol D, Sabanty W. Hepatitis B vaccination in preterm infants. Eur J Pediatr. 1999;158:293-297
11. Munoz A, Salvador A, Brodsky NL, Arbeter AM, Porat R. Antibody response of low birth weight infants to Haemophilus influenzae type b polyribosylribitol phosphate-outer membrane protein conjugate vaccine. Pediatrics. 1995;96:216-219
12. Kinney HC, Richerson GB, Dymecki SM, Darnall RA, Nattie EE. The brainstem and serotonin in the sudden infant death syndrome. Annu Rev Pathol. 2009;4:517-550
13. Deb S, Arrighi S. Potential effects of COVID-19 on cytochrome P450-mediated drug metabolism and disposition in infected patients. Eur J Drug Metab Pharmacokinet. 2021;46:185-203
14. Kearns G, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder J, Kauffman RE. Developmental pharmacology—drug disposition, action, and therapy in infants and children. New Engl J Med. 2003;349:1157-1167
15. Lu H, Rosenbaum S. Developmental pharmacokinetics in pediatric populations. J. Pediatr Pharmacol Ther. 2014;19:262-276
16. Dumas TE, Hawke RL, Lee CR. Warfarin dosing and the promise of pharmacogenomics. Cur Clin Pharmacol. 2007;2:11-21
17. Fortmann MI, Dirks J, Goedicke-Fritz S, Liese J, Zemlin M, Morbach H. et al. Immunization of preterm infants: Current evidence and future strategies to individualized approaches. Semin Immunopathol. 2022;44:767-784
18. Shaw CA, Li D, Tomljenovic L. Are there negative CNS impacts of aluminum adjuvants used in vaccines and immunotherapy? Immunotherapy. 2014;6:1055-1071
19. Abdel-Razzak Z, Loyer P, Fautrel A, Gautier JC, Corcos L, Turlin B. et al. Cytokines down-regulate expression of major cytochrome P-450 enzymes in adult human hepatocytes in primary culture. Mol Pharmacol. 1993;44:707-715
20. Aitken AE, Morgan ET. Gene-specific effects of inflammatory cytokines on cytochrome P450 2C, 2B6, and 3A4 mRNA levels in human hepatocytes. Drug Metab Dispos. 2007;35:1687-1693
21. McKee DM, Lofthouse S. Re-inventing traditional aluminum-based adjuvants: Insight into a new generation of aluminum salt-based adjuvants. Vaccine. 2024;42:3321-3332
22. Noe SM, Green MA, HogenEsch H, Hem SL. Mechanism of immunopotentiation by aluminum-containing adjuvants elucidated by the relationship between antigen retention at the inoculation site and the immune response. Vaccine. 2010;28:3588-3594
23. Zhao T, Cai Y, Jiang Y, He X, Wei Y, Yu Y. et al. Vaccine adjuvants: mechanisms and platforms. Signal Transduct Target Ther. 2023;8:283
24. Allegaert K, van de Velde M, van den Anker J. Neonatal clinical pharmacology. Paediatr Anaesth. 2014;24:30-38
25. US Department of Health & Human Services. April 28, 2021 Vaccine Ingredients. https://www.hhs.gov/immunization/basics/vaccine-ingredients/index.html
26. Evans WE, Relling MV. Pharmacogenomics: translating functional genomics into rational therapeutics. Science. 1999;286:487-491
27. Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Aluminum. U.S. Department of Health and Human Services, 2008. https://www.atsdr.cdc.gov/toxprofiles/tp22.pdf
28. Mitkus RJ, King DB, Hess MA, Forshee RA, Walderhaug MO. Updated aluminum pharmacokinetics following infant exposures through diet and vaccination. Vaccine. 2011;29:9538-9543
29. Physicians for Informed Consent. Aluminum in vaccines: What parents need to know. 2020. https://physiciansforinformedconsent.org/aluminum
30. Tulpule K, Dringen R. Formaldehyde in brain: an overlooked player in neurodegeneration? J Neurochem. 2013;127:7-21
31. Treluyer JM, Cheron G, Sonnier M, Cresteil T. Cytochrome P-450 expression in sudden infant death syndrome. Biochem Pharmacol. 1996;52:497-504
32. Prandota J. Possible pathomechanisms of sudden infant death syndrome: Key role of chronic hypoxia, infection /inflammation states, cytokine irregularities, and metabolic trauma in genetically predisposed infants. Am J Ther. 2004;11:517-546
33. Hunt CE, Brouillette RT. Sudden infant death syndrome: 1987 perspective. J Pediatr. 1987;110:669-678
34. Kinney HC, Randall LL, Sleeper LA, Willinger M, Belliveau R, Zec N. et al. Serotonergic brainstem abnormalities in Northern Plains Indians with the sudden infant death syndrome. J Neuropathol Exp Neurol. 2003;62:1178-1191
35. Paine SM, Jacques TS, Sebire NJ. Review: neuropathological features of unexplained sudden unexpected death in infancy: current evidence and controversies. Neuropathol Appl Neurobiol. 2014;40:364-384
36. Panigrahy A, Filiano J, Sleeper LA, Mandell F, Valdes-Dapena M, Krous HF. et al. Decreased serotonergic receptor binding in rhombic lip-derived regions of the medulla oblongata in the sudden infant death syndrome. J Neuropathol Exp Neurol. 2000;59:377-384
37. Ozawa Y, Takashima S. Developmental neurotransmitter pathology in the brainstem of sudden infant death syndrome: A review and sleep position. Forensic Sci Int. 2002;130(suppl):S53-S59
38. Machaalani R, Say M, Waters KA. Serotoninergic receptor 1A in the sudden infant death syndrome brainstem medulla and associations with clinical risk factors. Acta Neuropathol. 2009;117:257-265
39. Kashiwagi Y, Miyata A, Kumagai T, Maehara K, Suzuki E, Nagai T. et al. Production of inflammatory cytokines in response to diphtheria-pertussis-tetanus (DPT), haemophilus influenzae type b (Hib), and 7-valent pneumococcal (PCV7) vaccines. Hum Vaccin Immunother. 2014;10:677-685
40. Greenberg RG, Rountree W, Staat MA, Schlaudecker EP, Poindexter B, Trembath A. et al. Apnea after 2-month vaccinations in hospitalized preterm infants: A randomized clinical. JAMA Pediatr. 2025;179:246-254
41. Miller NZ. Vaccines and sudden Infant death: An analysis of the VAERS database 1990-2019 and review of the medical literature. Toxicology Reports. 2021;24:1324-1335
42. Boatmon v. Secretary of Health and Human Services. No. 13-611V. U.S. Court of Federal Claims, Office of Special Masters, 10 July 2017. https://ecf.cofc.uscourts.gov/cgi-bin/show_public_doc?2013vv0611-73-0
43. Ottaviani G, Lavezzi AM, Matturri L. Sudden infant death syndrome (SIDS) shortly after hexavalent vaccination: another pathology in suspected SIDS? Virchows Arch. 2006;448:100-104
44. Kuhnert R, Hecker H, Poethko-Müller C. et al. A modified self-controlled case series method to examine association between multidose vaccinations and death. Stat Med. 2011;30:666-677
45. Zinka B, Rauch E, Buettner A, Rueff F, Penning R. Unexplained cases of sudden infant death shortly after hexavalent vaccination. Vaccine. 2006;24:5779-5780
46. Eikelenboom-Schieveld SJM, Fogleman JC. Cytochrome P450 genes: Their role in drug metabolism and violence. In: Patel VB, ed. Handbook of Anger, Aggression, and Violence. Berlin, Germany: Springer. 2023:1-20
47. Koopmans AB, Braakman MH, Vinkers DJ. et al. Meta-analysis of probability estimates of worldwide variation of CYP2D6 and CYP3C19. Transl Psychiatry. 2021;11:141
48. Ingelman-Sundberg M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: The past, present and future. Trends Pharmacol Sci. 2004;25:193-200
49. Ganjare RS, Vagga AA, Dhok A, Anjankar A, Iha RK, Batulwar PS. Biochemical abnormalities associated with sudden infant death syndrome: a case report. Cureus. 2024;16:e55292
50. Mawson AR, Jacob B. Vaccination and neurodevelopmental disorders: A study of nine-year-old children enrolled in Medicaid. Science, Public Health Policy and the Law. 2025;6:2019-2025
51. Van Schaik RH. Dose adjustments based on pharmacogenetics of CYP450 enzymes. EJIFCC. 2008;19:42-47
52. Eliasson E, Wadelius M. Farmakogenomik - individuell anpassning av lakemedel ach das [Pharmacogenomics—a cornerstone of precision medicine]. Lakartidningen. 2021;118:20176
53. Abdelmonem BH, Abdelaal NM, Anwer EKE, Rashwan AA, Husein MA, Ahmed YF. et al. Decoding the Role of CYP450 Enzymes in Metabolism and Disease: A Comprehensive Review. Biomedicines. 2024;12:1467
Author biography
Gary S. Goldman, PhD, currently serves as an independent computer scientist and consultant specializing in epidemiological studies and vaccine safety. He served as the Research Analyst for the Varicella Active Surveillance project (VASP) in collaboration with the Centers for Disease Control and Prevention (CDC), where he investigated the impact of the varicella vaccination program on the closely related herpes zoster epidemiology and utilized capture-recapture statistical methods. Goldman is founder and former Editor-in-Chief of Medical Veritas, a peer-reviewed publication that has been cited in numerous medical-legal litigation involving alleged cases of Shaken Baby Syndrome, providing alternative medical perspectives considered in court proceedings. His work continues to influence discussions on vaccine policy and public health.
Richard Z. Cheng, MD, PhD, is a U.S.-based, board-certified physician specializing in integrative orthomolecular medicine. He serves as Editor-in-Chief of the Orthomolecular Medicine News Service and is a Hall of Fame inductee of the International Society for Orthomolecular Medicine. Dr. Cheng works internationally as a consultant and educator, with clinical interests in orthomolecular, functional, anti-aging, and low-carbohydrate medicine. He is the founder of Cheng Integrative Health and co-founder of the Low Carb Medicine Alliance of China. His work focuses on reversing chronic diseases through root-cause strategies including diet, nutrition, detoxification, hormone therapy, and regenerative medicine.
![]() Corresponding author: Gary S. Goldman, Independent Researcher, Email: pearblossominccom, Tel.: +1 661-305-2310.
Corresponding author: Gary S. Goldman, Independent Researcher, Email: pearblossominccom, Tel.: +1 661-305-2310.

 Global reach, higher impact
Global reach, higher impact