3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(5):896-903. doi:10.7150/ijms.87941 This issue Cite
Research Paper
Prediction of outcomes for rescue cerclage in cervical insufficiency: A multicenter retrospective study
1. Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, 06591 Seoul, Republic of Korea.
2. Department of Anesthesiology and Pain Medicine, Eunpyeong St. Mary's Hospital College of Medicine, The Catholic University of Korea, 06591 Seoul, Republic of Korea.
3. Department of Obstetrics and Gynecology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, 06591 Seoul, Republic of Korea.
*These authors contributed equally to this work and share first authorship.
Abstract
Purpose: Cervical insufficiency is a significant risk factor for preterm birth and miscarriage during the second trimester; cervical cerclage is a treatment option. This study seeks to evaluate the predictive roles of various clinical factors and to develop predictive models for immediate and long-term outcomes after rescue cerclage.
Methods: We conducted a multicenter retrospective study on patients who underwent rescue cerclage at 14 to 26 weeks of gestation. Data were collected from the Electronic Medical Record systems of participating hospitals. Outcomes were dichotomized into immediate failure (inability to maintain pregnancy for at least 48 hours post-cerclage, gestational latency < 2 days) and long-term success (maintenance of pregnancy until at least 28 weeks of gestation). Clinical factors influencing these outcomes were analyzed.
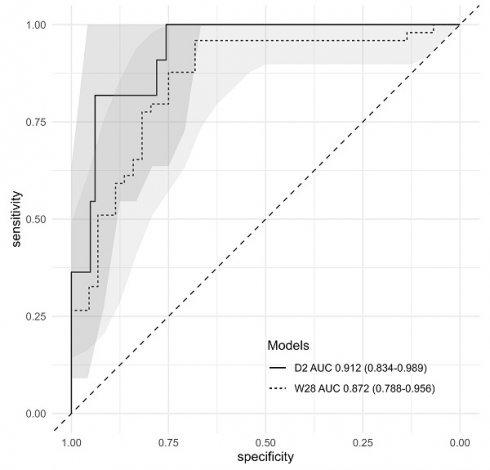
Results: The study included 98 patients. Immediate failure correlated with longer prolapsed membrane lengths, elevated C-reactive protein levels at admission, and extended operation time. The successful maintenance of pregnancy until at least 28 weeks was associated with earlier gestational age at diagnosis, negative AmniSure test results, longer lengths of the functional cervix, and smaller cervical dilatation at the time of cerclage. Binary logistic regression models for immediate failure and long-term success exhibited excellent and good predictive abilities, respectively (AUROC = 0.912, 95% CI: 0.834-0.989; and AUROC = 0.872, 95% CI: 0.788-0.956).
Conclusion: The developed logistic regression models offer a valuable tool for the prognostic assessment of patients undergoing rescue cerclage, enabling informed clinical decision-making.
Keywords: cervical insufficiency, cerclage, rescue cerclage, predictive model, preterm birth, outcome, prognosis

 Global reach, higher impact
Global reach, higher impact