3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(5):809-816. doi:10.7150/ijms.94485 This issue Cite
Review
Role of mitochondria in doxorubicin-mediated cardiotoxicity: from molecular mechanisms to therapeutic strategies
1. First Afliated Hospital, Heilongjiang University of Chinese Medicine, Harbin 150040, China.
2. Brandeis University, Waltham, MA 02453, USA.
3. Heilongjiang University of Chinese Medicine, Harbin 150040, China.
4. Department of Cardiology, Guang'anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, 100053, China.
Abstract
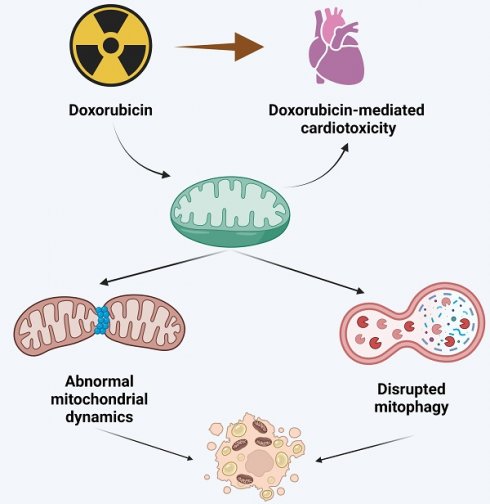
This comprehensive review delves into the pivotal role of mitochondria in doxorubicin-induced cardiotoxicity, a significant complication limiting the clinical use of this potent anthracycline chemotherapeutic agent. Doxorubicin, while effective against various malignancies, is associated with dose-dependent cardiotoxicity, potentially leading to irreversible cardiac damage. The review meticulously dissects the molecular mechanisms underpinning this cardiotoxicity, particularly focusing on mitochondrial dysfunction, a central player in this adverse effect. Central to the discussion is the concept of mitochondrial quality control (MQC), including mitochondrial dynamics (fusion/fission balance) and mitophagy. The review presents evidence linking aberrations in these processes to cardiotoxicity in doxorubicin-treated patients. It elucidates how doxorubicin disrupts mitochondrial dynamics, leading to an imbalance between mitochondrial fission and fusion, and impairs mitophagy, culminating in the accumulation of dysfunctional mitochondria and subsequent cardiac cell damage. Furthermore, the review explores emerging therapeutic strategies targeting mitochondrial dysfunction. It highlights the potential of modulating mitochondrial dynamics and enhancing mitophagy to mitigate doxorubicin-induced cardiac damage. These strategies include pharmacological interventions with mitochondrial fission inhibitors, fusion promoters, and agents that modulate mitophagy. The review underscores the promising results from preclinical studies while advocating for more extensive clinical trials to validate these approaches in human patients. In conclusion, this review offers valuable insights into the intricate relationship between mitochondrial dysfunction and doxorubicin-mediated cardiotoxicity. It underscores the need for continued research into targeted mitochondrial therapies as a means to improve the cardiac safety profile of doxorubicin, thereby enhancing the overall treatment outcomes for cancer patients.
Keywords: doxorubicin, cardiotoxicity, mitochondria, mitochondrial quality control

 Global reach, higher impact
Global reach, higher impact