3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2024; 21(3):530-539. doi:10.7150/ijms.88519 This issue Cite
Research Paper
How to Defeat Multidrug-Resistant Bacteria in Intensive Care Units. A Lesson from the COVID-19 Pandemic. Prevention, Reservoirs, and Implications for Clinical Practice
1. Department of Nursing and Midwifery, Wroclaw Medical University, Wroclaw, Poland.
2. Department of Anaesthesiology and Intensive Therapy, Hospital of Ministry of the Interior and Administration, Wroclaw, Poland.
3. Department of Anaesthesiology and Intensive Therapy, Wroclaw Medical University, Wroclaw, Poland.
4. Department of Microbiology, Wroclaw Medical University, Wroclaw, Poland.
5. Department of Laboratory Diagnostics, 4th Military Clinical Hospital, Wroclaw, Poland.
6. Department of Pharmaceutical Microbiology and Parasitology, Wroclaw Medical University, Wroclaw, Poland.
Abstract
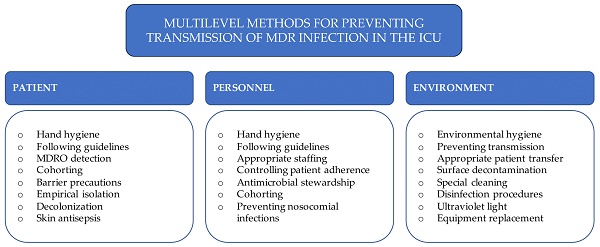
Background: Intensive care unit (ICU) patients are at high risk of infection due to multiple invasive procedures, malnutrition, or immunosuppression. The rapid increase in infections with multidrug-resistant organisms (MDRO) during the COVID-19 pandemic caused a dilemma, as the rules of the sanitary regime in ICU rooms were strictly adhered to in the prevailing epidemiological situation. The combat to reduce the number of infections and pathogen transmission became a priority for ICU staff. This study aimed to assess whether eliminating environmental reservoirs and implementing improved procedures for patient care and decontamination and washing equipment in the ICU reduced the incidence of infections caused by MDR strains.
Material and methods: The study retrospectively analyzed data in the ICU during the COVID-19 pandemic. The samples were collected based on microbiological culture and medical records in the newly opened ICU (10 stations) and hospital wards where COVID-19 patients were hospitalized. Environmental inoculations were performed during the COVID-19 pandemic every 4-6 weeks unless an increase in the incidence of infections caused by MDR strains was observed. Through microbiological analysis, environmental reservoirs of MDR pathogens were identified. The observation time was divided into two periods, before and after the revised procedures. The relationship between isolated strains of Klebsiella pneumoniae NDM from patients and potential reservoirs within the ICU using ERIC-PCR and dice methods was analyzed.
Results: An increased frequency of infections and colonization caused by MDRO was observed compared to the preceding years. A total of 23,167 microbiological tests and 6,985 screening tests for CPE and MRSA bacilli were collected. The pathogen spread was analyzed, and the findings indicated procedural errors. Assuming that the transmission of infections through the staff hands was significantly limited by the restrictive use of personal protective equipment, the search for a reservoir of microorganisms in the environment began. MDR strains were grown from the inoculations collected from the hand-wash basins in the wards and from inside the air conditioner on the ceiling outside the patient rooms. New types of decontamination mats were used in high-risk areas with a disinfectant based on Glucoprotamine. Active chlorine-containing substances were widely used to clean and disinfect surfaces.
Conclusions: Infections with MDR strains pose a challenge for health care. Identification of bacterial reservoirs and comprehensive nursing care significantly reduce the number of nosocomial infections.
Keywords: COVID-19, drug resistance, bacterial, molecular epidemiology, mortality, primary prevention

 Global reach, higher impact
Global reach, higher impact