3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2023; 20(11):1508-1512. doi:10.7150/ijms.86933 This issue Cite
Research Paper
The obesity paradox in Japanese COVID-19 patients
1. Infection Control Committee, Shimonoseki City Hospital, Shimonoseki, Japan.
2. Department of Anesthesiology, Shimonoseki City Hospital, Shimonoseki, Japan.
3. Department of Medicine and Biosystemic Science, Kyushu University Graduate School of Medical Sciences, Fukuoka, Japan.
Abstract
Purpose: To investigate the effect of obesity on mortality and invasive respiratory care (IRC) in patients with COVID-19.
Methods: We studied 1,105 patients for 34 months and collected data. The primary outcome was all-cause death at 29 days. The secondary outcome was IRC indicated by a pulse oximetry rate below 93% at a mask oxygenation rate of 5 L/min or more.
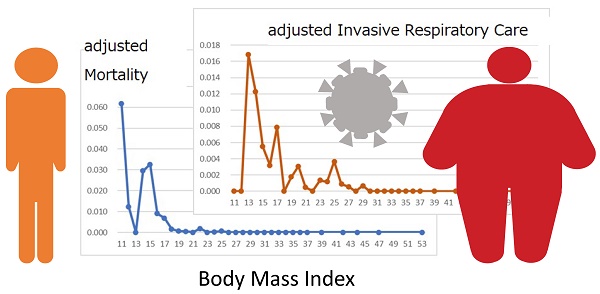
Results: Age- and sex-adjusted multivariate regression analysis for 29-day deaths showed the significance of body mass index (BMI) > 19.6 kg/m2 (odds ratio 0.117, 95% confidence interval 0.052-0.265, P<0.001). The graphs with BMI in the abscissa showed, within a BMI between 11 and 25 kg/m2, a decreasing pattern for mortality and IRC rate, and no increase in overweight.
Conclusion: In Japanese COVID-19 patients, the risk of mortality and the IRC rate decreased in underweight patients and remained low in overweight patients, suggesting the importance of the obesity paradox.
Keywords: risk, SARS-CoV-2, high flow nasal cannula oxygenation, chemotherapy

 Global reach, higher impact
Global reach, higher impact