ISSN: 1449-1907
Int J Med Sci 2022; 19(14):1989-1994. doi:10.7150/ijms.78182 This issue Cite
Research Paper
Prognostic value of pretreatment systemic inflammatory markers in patients with stage I endometrial cancer
1. Department of Obstetrics and Gynecology, Yonsei University Wonju College of Medicine, Republic of Korea.
2. Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
3. Department of Obstetrics and Gynecology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
Abstract
Objective: Evaluate the prognostic value of monocyte-lymphocyte ratio (MLR) in patients with stage I endometrial cancer.
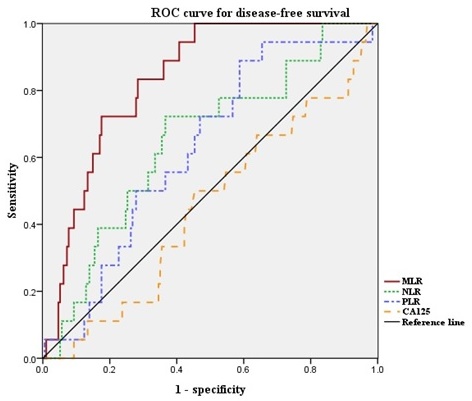
Method: Data from 225 patients with stage I endometrioid endometrial cancer who underwent surgical resection between January 2010 and December 2020 were reviewed. The receiver operating characteristic (ROC) curves were generated for the neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and MLR. Optimal cut-off values were determined as the points at which the Youden index (sensitivity + specificity - 1) was maximal. Based on the results of the ROC curve analysis, the patients were grouped into high MLR and low MLR groups. Recurrence rate, and disease-free survival were compared between the two groups. The prognostic factors were investigated using univariate and multivariate Cox proportional hazards model.
Results: The optimal cut-off value of MLR was 0.220 (AUC, 0.835; p < 0.001). Significantly more patients in the high MLR group experienced recurrence (20.3% vs. 1.9%, p < 0.0001). In multivariate analysis, grade, depth of myometrial invasion, adjuvant RT, and high MLR were independent prognostic factors for disease-free survival.
Conclusion: Elevated MLR was significantly associated poor clinical outcomes in patients with stage I endometrioid endometrial cancer. Our findings suggest that MLR may be clinically reliable and useful as an independent prognostic marker for patients with stage I endometrioid endometrial cancer.
Keywords: endometrial cancer, uterine cancer, systemic inflammation reponse, adverse risk factors, monocyte-lymphocyte ratio

 Global reach, higher impact
Global reach, higher impact