Impact Factor
ISSN: 1449-1907
Int J Med Sci 2013; 10(2):198-205. doi:10.7150/ijms.5248 This issue Cite
Research Paper
Statins Therapy Can Reduce the Risk of Atrial Fibrillation in Patients with Acute Coronary Syndrome: A Meta-Analysis
1. Department of Cardiology, Children's Hospital of Chongqing Medical University, Chongqing, P. R. China.
2. Department of Cardiology, The Second Affiliated Hospital, Chongqing Medical University, Chongqing, P.R.China.
* Xue Zhou and Jian-lin Du made the same contribution to this paper.
Received 2012-9-18; Accepted 2012-12-28; Published 2013-1-10
Abstract
Background: It is a controversy whether statins therapy could be beneficial for the occurrence of atrial fibrillation (AF) in acute coronary syndrome (ACS). To clarify this problem, we performed a meta-analysis with the currently published literatures.
Methods: The electronic databases were searched to obtain relevant trials which met the inclusion criteria through October 2011. Two authors independently read the trials and extracted the related information from the included studies. Either fixed-effects models or random-effects models were assumed to calculate the overall combined risk estimates according to I2 statistic. Sensitivity analysis was conducted by omitting one study in each turn, and publication bias was evaluated using Begg's and Egger's test.
Results: Six studies were eligible to inclusion criteria, of the six studies, 161305 patients were included in this meta-analysis, 77920 (48.31%) patients had taken the statins therapy, 83385 (51.69%) patients had taken non-statins therapy. Four studies had investigated the effect of statins therapy on occurrence of new-onset AF in ACS patients, another two had described the association between statins therapy and occurrence of AF in ACS patients with AF in baseline. The occurrence of AF was reduced 35% in statins therapy group compared to that in non-statins group (95% confident interval: 0.55-0.77, P<0.0001), and the effect of statins therapy seemed more beneficial for new-onset AF (RR=0.59, 95%CI: 0.48-0.73, p=0.096) than secondary prevention of AF (RR=0.70, 95%CI: 0.43-1.14, p=0.085). There was no publication bias according to the Begg's and Egger's test (Begg, p=0.71; Egger, p=0.73).
Conclusion: Statins therapy could reduce the risk of atrial fibrillation in patients with ACS.
Keywords: statins, atrial fibrillation, acute coronary syndrome.
Introduction
Atrial fibrillation (AF) is a common arrhythmia associated with acute coronary syndrome (ACS) and the estimates were up to 20% in acute myocardial infarction (AMI) patients [1-4]. The ACS patients developed AF may have poor prognosis. Previous studies had showed that ACS patients associated with AF may have longer in-hospital duration, higher rates of stroke, and increase the short and long-term mortality [2, 4-7]. Therefore, the treatment or prevention of AF may improve the prognosis in ACS patients. Accumulating evidences have been demonstrated that statins, hydroxymethylglutary-CoA reductase inhibitors, can reduce the incidence of AF in coronary artery disease (CAD) patients [8-10], nevertheless other studies showed that statins therapy was nearly no beneficial to prevent AF in patients with acute coronary disease [11], isolated coronary artery bypass grafting [12], undergoing cardiac surgery [13]. In order to elucidate whether statins are beneficial to ACS patients complicated with AF, we performed a meta-analysis to clarify this problem through analyzing the currently published literatures.
Methods
Retrieval strategy
In order to obtain relevant trials, we searched through EMbase, PubMed, Medline, ISI Web of Science for all cohort studies or randomized controlled trials through October 2011, using the following terms: statins, hydroxymethylglutary-CoA reductase inhibitors, HMG-CoA reductase inhibitors, lipid lowering therapy, coronary disease, coronary heart disease, coronary artery disease, acute coronary syndrome, ACS, atrial fibrillation, AF. The retrieval strategies were presented in table 1 with restrictions to English language studies only. We also manually searched the relevant studies from related review articles and meta-analyses.
Retrieval strategies
| Pubmed | #1 statins |
| #2 hydroxymethylglutary-CoA reductase inhibitors | |
| #3 HMG-CoA reductase inhibitors | |
| #4 lipid lowering therapy | |
| #5 #1 or #2 or #3 or #4 | |
| #6 atrial fibrillation | |
| #7 AF | |
| #8 #6 or #7 | |
| #9 coronary disease | |
| #10 coronary heart disease | |
| #11 coronary artery disease | |
| #12 acute coronary syndrome | |
| #13 ACS | |
| #14 #9 or #10 or #11 or #12 or #13 | |
| #15 #5 and #8 and #14 | |
| ISI Web of Science, Medline, Embase | #1 statins or hydroxymethylglutary-CoA reductase inhibitors or HMG-CoA reductase inhibitors or lipid lowering therapy |
| #2 atrial fibrillation or AF | |
| #3 coronary disease or coronary heart disease or coronary artery disease or acute coronary syndrome or ACS | |
| #4 #1 and #2 and #3 |
Note: We searched the references according to the sequence of the number.
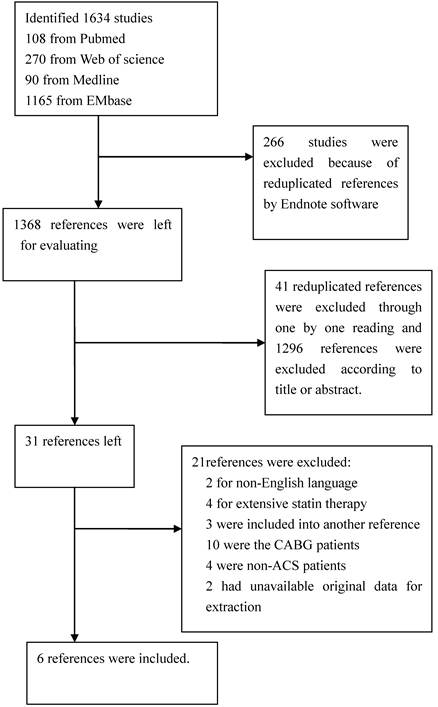
With these key words, 1634 abstracts were retrieved. Full text reviews were obtained when the studies had possible relevance to this study. For the unavailable data, we did not contact the authors.
Study selection
We firstly excluded the reduplicated studies using Endnote software, then screened the studies according to the titles or abstracts. The second screening was preformed based on the full-text reviews. We looked for the studies that met all the specific criteria: (1) the study design was cohort study or randomized controlled trial; (2) the study subjects were the patients with acute coronary syndrome; (3) patients with statins therapy compared to those with non-statins therapy; (4) clinical outcome was occurrence or new-onset atrial fibrillation; (5) the data for extraction in the original article were available. Articles were excluded if they met one of the following criteria: (1) acute coronary syndrome patients with extensive or high dose statins therapy compared to those with traditional statins therapy; (2) patients who were under coronary artery bypass grafting or coronary artery disease; (3) reviews. If one trial had published two or more publications with different durations, we would choose the publication with the longest duration. Two authors (Xue Zhou and Jia Yuan) independently read the titles, abstracts, and/or full texts to determine whether they were satisfied with the inclusion/exclusion criteria (figure 1). For the disagreement or uncertainty, we got to resolve by discussion or consensus of a third reviewer.
Data extraction
The key exposure variable was the presence (statins therapy group) or absence of statin use (non-statins therapy group) at baseline.
The quality of the non-randomized studies was assessed by using the Newcastle-Ottawa Scale (NOS) with slight modification [14]. The quality of the studies was evaluated by examining three items: patient selection, comparability and assessment of outcome (Table 2).
The data extraction was performed independently more than twice by two authors (Xue Zhou and Jianlin Du) in order to get the exact information. The following information were extracted from each retrieved article: first author, year, study population, women, design, type of statin, endpoint type of AF, duration, total patients (patients in statin group/non-statin group), the total incidence of AF(patients in statin group/ non-statin group), Diabetes Mellitus, heart failure, renal insufficiency, hyperlipidemia, hypertension, ACEI or ARB, beta-blocker (Table 3). For the disagreement or uncertainty, it was resolved by consensus.
Statistical analysis
Relative ratio (RR) was used to measure the effect size. Heterogeneity test was performed using I2 statistic, which is a quantitative measure of inconsistency across studies [15]. Pooled RR were calculated for statins therapy group versus non-statins therapy group, using either fixed-effects models or random-effects models according to I2 statistic, if I2 is less than 50%, we would choose fixed-effects models; otherwise the random-effects models would be used. The 95% confident interval(CI) was also calculated. Sensitivity analysis was conducted by omitting one study in each turn in order to investigate the influence of a single study on the overall risk estimate and test the stability of the results. Publication bias was evaluated using Begg's and Egger's test. All statistical analyses were performed using STATA version 11.0 (StataCorp LP, College Station, Texas). A p value<0.05 was considered statistically significant, except where otherwise specified.
Check List for Quality Assessment and Scoring of Nonrandomized Studies
| Check list |
|---|
| Selection |
| 1. The exposed cohort was truly or somewhat representative of the average described in the community? (If yes, one star) |
| 2. The non-exposed cohort was drawn from the same community as the exposed cohort? (If yes, one star) |
| 3. The exposure was ascertained through secure record or structured interview? (If yes, one star) |
| 4. The outcome of interest was not present at start of study? (If yes, one star) |
| Comparability |
| 1. Group comparable for statins therapy. (If yes, one star) |
| 2. Group comparable for age, gender, medical history (such as diabetes mellitus, hypertension, hyperlipidemia, prior treatments). (If yes, one star) |
| Outcome assessment |
| 1. Assessment of outcome. (If outcome was independent blind assessment, one star) |
| 2. Adequacy of follow-up. (One star if follow-up>95%) |
The characteristics of the included studies in the meta-analysis
| Ramani[16] | Vedre [17] | Dachin [18] | Dziewierz[19] | Ozaydin[20] | Bang* [21] | |
|---|---|---|---|---|---|---|
| Year | 2007 | 2009 | 2010 | 2010 | 2010 | 2011 |
| Study population | ACS/NSTEMI | NSTEMI/STEMI/UA | NSTEMI/STEMI | NSTEMI/STEMI/UA | NSTEMI/STEMI/UA | MI |
| Women | 52(3.41%) | 21340(33.00%) | 1056(31.1%) | 461(46.1%) | 245(24.5%) | N/A |
| Design | retrospective | prospective multinational | prospective multicentre | prospective Multicentre | prospective | prospective |
| Type of statins# | simvastatin | any type | rosuvastatin atorvastatin | any type | 154atorvastatin,27fluvastatin,10 pravastatin,9rosuvastatin,41 simvastatin fluvastatin 10 pravastatin 9 rosuvastatin 41 simvastatin | any type |
| Endpoint-type of AF | new-onset AF | recurrence AF | new-onset AF | new-onset AF | recurrence AF | new-onset AF |
| Duration(year) | 4.1 | 8 | 5 | 1 | 3 | 10 |
| Total patients | 1526 | 64679 | 3396 | 1001 | 1000 | 89703 |
| Statin group | 601 | 17636 | 2551 | 847 | 241 | 56044 |
| Non-statin group | 925 | 47043 | 845 | 154 | 759 | 33659 |
| The incidence of AF | 10.80% | 7.78% | 4.68% | 2.40% | 8.80% | 11.94% |
| Statin group | 6.80% | 6.90% | 3.90% | 1.89% | 5% | 10.00% |
| Non-statin group | 13.30% | 8.20% | 7.00% | 5.20% | 10% | 15.00% |
| Diabetes Mellitus | 39.84% | 24.90% | 35.48% | 23.38% | 23.60% | N/A |
| Heart Failure | 17.63% | 10.13% | 5.04% | 23.88% | 5.90% | N/A |
| Hyperlipidemia | 50.26% | 48.02% | N/A | 57.54% | N/A | N/A |
| Renal insufficiency | N/A | 7.55% | 5.48% | 6.00% | 0.50% | N/A |
| Hypertension | 69.40% | 61.66% | 45.67% | 78.92% | 55% | N/A |
| ACEI or ARB | 42.60% | 64.71% | N/A | 75.52% | 29.10% | N/A |
| beta-blocker | 55.90% | 82.20% | N/A | 80.72% | 26.40% | N/A |
Note: 1.*just abstract available. 2. ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; N/A: non-available; NSTEMI: non-ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction; UA: unstable angina pectoris. 3.# The dose of statins was not available.
Flow chart showing the process of screening references.
Results
A meta-analysis with data derived from six cohort studies, which applying with statins in patients with ACS or suspected ACS for preventing atrial fibrillation, was conducted. The endpoint was occurrence or new-onset AF. Among the six references, five references were full-text reviews and another one was abstract. Four studies had investigated the effect of statins therapy on occurrence of new-onset AF in ACS patients, another two had described the association between statins therapy and occurrence of AF in ACS patients without AF free in baseline. Of the six eligible trials, 161305 patients were included in this meta-analysis, 77920 (48.31%) patients had taken the statins therapy, 83385 (51.69%) patients had taken non-statins therapy. All six trials reported AF outcomes. Incidence or recurrence of AF occurred in 16176 patients: 7070 of 77920 in patients treated with statins versus 9106 of 83385 in control subjects. The characteristics of these included studies were presented in table 3 and the quality assessment was performed according to NEWCASTLE - OTTAWA QUALITY ASSESSMENT SCALE (Table 4).
Assessment of quality of included studies
| Study | Selection | Comparability | Outcome | Score |
|---|---|---|---|---|
| Ramani[16] | ★★★ | ★★ | ★★ | ★★★★★★★ |
| Vedre[17] | ★★★ | ★★ | ★★ | ★★★★★★★ |
| Dachin[18] | ★★★★ | ★★ | ★★ | ★★★★★★★★ |
| Dziewierz[19] | ★★★★ | ★★ | ★ | ★★★★★★★★ |
| Ozaydin[20] | ★★★ | ★★ | ★★ | ★★★★★★★ |
Note: For the study by Bang C.N. was only abstract available, we did not get further to assess the quality.
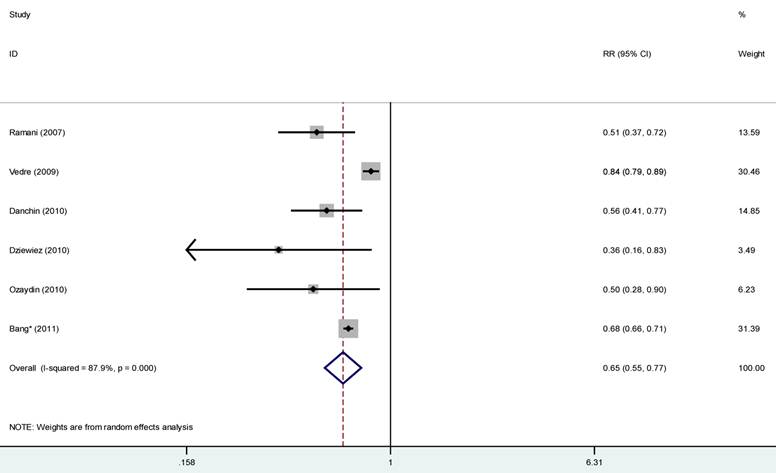
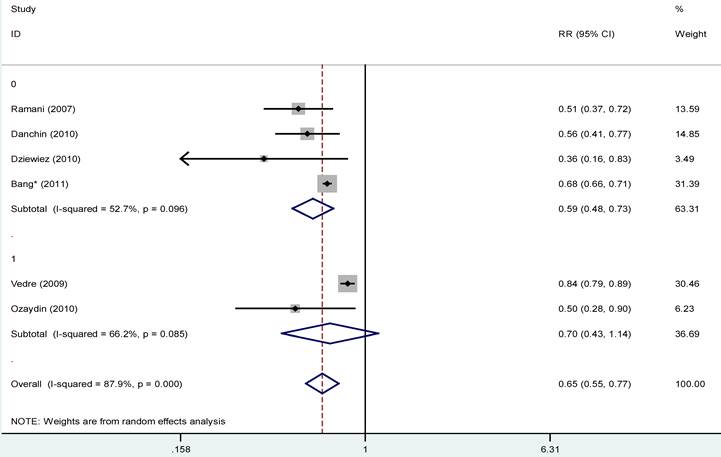
The occurrence of AF was reduced 35% in statins therapy group compared to that in non-statins group (95% confident interval: 0.55-0.77, P<0.0001) with high heterogeneity (I2=87.9%, p<0.01), therefore we assumed random-effects models (Fig 2). After we omitted the study with abstract available, the remaining studies showed the similar results (OR 0.58, 95%CI: 0.42-0.80; p=0.001), with substantial evidence of heterogeneity (I2=79.6%) (Fig 3). The effect of statins therapy seemed more beneficial for new-onset AF (RR=0.59, 95%CI: 0.48-0.73, p=0.096) than secondary prevention of AF (RR=0.70, 95%CI: 0.43-1.14, p=0.085) (Fig 4). In order to explore potential sources of heterogeneity and test the stability of the results, we performed sensitivity analysis by excluding any single study, and the result did not materially alter the overall combined RR, with a range from 0.58 (95%CI: 0.42 to 0.80; p=0.001) to 0.68 (95%CI: 0.57 to 0.81; p<0.001). Publication bias was evaluated using Begg's and Egger's test, and there was no publication bias among the include studies (Begg, p=0.71; Egger, p=0.73).
Statins and the risk of atrial fibrillation (AF). Forest funnel showed the association of statins therapy and the risk of AF in patients presented with acute coronary syndrome with random-effects model. RR=relative ratio; CI=confidence interval.
Statins and the risk of atrial fibrillation. Studies with only abstract available were excluded from this analysis, and forest funnel showed the association of statins therapy and the risk of AF in patients presented with acute coronary syndrome. Abbreviations as in figure 2.

Subgroup analysis was conducted according to the type of AF, and forest funnel showed the association of statins therapy and the occurrence of AF in patients presented with acute coronary syndrome. 0= new-onset AF group, and 1 = recurrence AF group. Abbreviations as figures 2 and 3.
Discussion
This meta-analysis derived from six cohort studies suggested that statins therapy was associated with a 35% reduction in the risk of new-onset or recurrence AF in patients with ACS compared to those with non-statins therapy, after we excluded the study with only abstract available, the beneficial effect was nearly the same. The reduction effect seemed more advantageous in the prevention of new-onset AF than in the prevention of recurrence AF.
For the subject with no restriction of CHD, a previous meta-analysis by Rahimi K showed that statins therapy had no evidence of a reduction in the risk of atrial fibrillation [22]. For the CHD patients, the impact of statins therapy on prevention AF was conflicting. The MIRACL trial demonstrated that statins use was nearly no beneficial to prevent AF in patients with acute coronary disease (OR 0.97, 95%CI: 0.72-1.31) [11], statins therapy was not associated with a decrease in the risk of AF in patients after coronary artery bypass grafting [23], in patients with CHD [24]. While some studies had showed statins therapy could reduce the risk of AF in patients with CHD [8-10]. And the present meta-analysis, which demonstrated statins therapy would decrease the risk of new-onset or recurrence AF in patients with ACS, might be more credible for its large subjects, and may provide some advice to the clinical practice. Therefore, the effect of statins therapy on preventing AF is not beneficial to patients with no restriction, and is conflicting in CHD patients, but is beneficial to ACS patients in the present meta-analysis.
The underlying mechanism behind the protective effects of statin on the risk of developing AF in CHD patients is unclear. Both AF and CHD are an inflammatory condition in which myeloperoxidase (MPO) is known to play a significant role [25, 26]. What is more, in the condition of AF or CHD, patients have increased C-reactive protein (CRP) levels in their blood [27, 28], the concentration of CRP in the blood seems to be associated with the total amount of time that patient experiences AF [29] and directly correlate with adverse effects in CHD patients. Statins can inhibit interleukin-6 (IL-6) and tumor necrosis factor α (TNF-α) production and nuclear factor kappa B (NF- κB) activation, and are anti-inflammatory in nature [30], and they may decrease the production of MPO and MPO-accompanied fibrosis and initiation and progression of AF and atherosclerosis. A systematic literature written by Oliver Adam [31] and a research reported by Reilly SN [32] showed statins can play a role in antiarrhythmic effects through improving endothelial nitric oxide (NO) availability and reducing inflammation, oxidative stress, and neurohormonal activation.
Source of heterogeneity
The heterogeneity was observed in the present meta-analysis, sensitivity analysis by omitting every single study was performed to explore the potential source of heterogeneity, but the result did not materially alter the overall combined RR, which means our results are stable. The meta-regression on sample size was performed for the sample size in present meta-analysis ranges from 1000 to 89703, whereas the result showed the sample-size was not the source of heterogeneity (p=0.138). The baseline characteristics of subjects may result in heterogeneity in present meta-analysis: (1)underlying disease associated with heart is an important factor to affect the incidence of AF, for heart related basic disease may lead to the changes of heart structure, which may influence the electrophysiology of heart; (2)the gender is another an important factor, for aged-female is much easier to have CAD and the prognosis may be more poor than aged-male, whereas the amount of women in included studies changes quite a lot, and this may lead to heterogeneity; (3) the basic treatments could also affect the heterogeneity.
Limitations
It is noteworthy that the results of the study by Bang et al. [21] have not been published in a full text review to date. However results were similar when the study [21] was not included in the present analysis. The substantial heterogeneity was observed in our meta-analysis, although sensitivity analysis and meta-regression were conducted to detect the source of heterogeneity, we could not identify the exact source of heterogeneity. Only GRACE study reported by Vedre et al. [17] had study the effect of statins therapy on death, cardiac arrest, ventricular fibrillation in patients with ACS, the majority of studies included in present meta-analysis were focus on the occurrence of AF, so it is unclear whether the early statins therapy in ACS patients could really improve the prognosis or not, and need more studies to clarify. We do not study the effect of different type and/or does of statins on prevention AF in ACS patients, for the type and/or does of statins in some studies were unclear, we could not make further efforts to identify the association between type and/or does of statins and AF.
Conclusion
The statins therapy was associated with a 35% reduction in the risk of new-onset or recurrence AF in patients with ACS compared to those with non-statins therapy, and the beneficial effect may more marked in prevention new-onset AF than in prevention recurrence AF.
Acknowledgements
This study was partly supported by grants from the National Natural Science Foundation of China (No.81070140) and the project of Chongqing Health Administration (No.2008-2-45).
Competing Interests
The authors guaranteed that there are no competing interests within this work.
References
1. Goldberg RJ, Seeley D, Becker RC. et al. Impact of atrial fibrillation on the in-hospital and long-term survival of patients with acute myocardial infarction: A community-wide perspective. Am Heart J. 1990;119:996-1001
2. Pedersen OD, Bagger H, Køber L. et al. on behalf of the TRACE Study group. The occurrence and prognostic significance of atrial fibrillation/flutter following acute myocardial infarction. Eur Heart J. 1999;20:748-754
3. Rathore SS, Berger AK, Weinfurt KP. et al. Acute myocardial infarction complicated by atrial fibrillation in the elderly: prevalence and outcomes. Circulation. 2000;101:969-974
4. Pizzetti F, Turazza FM, Franzosi MG. et al. on behalf of the GISSI-3 Investigators. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart. 2001;86:527-532
5. Mehta RH, Dabbous OH, Granger CB. et al. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am J Cardiol. 2003;92:1031-6
6. Lopes RD, Pieper KS, Horton JR. et al. Short- and long-term outcomes following atrial fibrillation in patients with acute coronary syndromes with or without ST-segment elevation. Heart. 2008;94:867-873
7. Berton G, Cordiano R, Cucchini F. et al. Atrial fibrillation during acute myocardial infarction: Association with all-cause mortality and sudden death after 7-year of follow-up. Int J Clin Pract. 2009;63:712-721
8. Young-Xu Y, Jabbour S, Golderg R. et al. Usefulness of statin drugs in protecting against atrial fibrillation in patients with coronary artery disease. Am J Cardiol. 2003;92:1379-1383
9. Pellegrini CN, Vittinghoff E, Lin F. et al. Statin use is associated with lower risk of atrial fibrillation in women with coronary disease: the HERS trial. Heart. 2009;95:704-708
10. Kulik A, Singh JP, Levin R. et al. Association Between Statin Use and the Incidence of Atrial Fibrillation Following Hospitalization for Coronary Artery Disease. Am J Cardiol. 2010;105:1655-1660
11. Schwartz GG, Olsson AG, Chaitman B. et al. Effect of intensive statin treatment on the occurrence of atrial fibrillation after acute coronary syndrome: an analysis of the MIRACL trial. Circulation. 2004;110(Suppl):S740
12. Subramaniam K, Koch CG, Bashour A. et al. Preoperative statin intake and morbid events after isolated coronary artery bypass grafting. J Clin Anesth. 2008;20:4-11
13. Virani SS, Nambi V, Razavi M. et al. Preoperative statin therapy is not associated with a decrease in the incidence of postoperative atrial fibrillation in patients undergoing cardiac surgery. Am Heart J. 2008;155:541-546
14. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Wells GA, Shea B, O'Connell D, et al. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
15. Higgins JP, Thompson SG, Deeks JJ. et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60
16. Ramani G, Zahid M, Good CB. et al. Comparison of frequency of new-onset atrial fibrillation or flutter in patients on statins versus not on statins presenting with suspected acute coronary syndrome. Am J Cardiol. 2007;100:404-405
17. Vedre A, Gurm HS, Froehlich JB, et al; GRACE Investigators. Impact of Prior Statin Therapy on Arrhythmic Events in Patients With Acute Coronary Syndromes (from the Global Registry of Acute Coronary Events [GRACE]). Am J Cardiol. 2009;104:1613-7
18. Danchin N, Fauchier L, Marijon E. et al. Impact of early statin therapy on development of atrial fibrillation at the acute stage of myocardial infarction: Data from the FAST-MI register. Heart. 2010;96:1809-14
19. Dziewierz A, Siudak Z, Rakowski T. et al. Prognostic significance of new onset atrial fibrillation in acute coronary syndrome patients treated conservatively. Cardiol J. 2010;17:57-64
20. Ozaydin M, Turker Y, Erdogan D. et al. The association between previous statin use and development of atrial fibrillation in patients presenting with acute coronary syndrome. Int J Cardiol. 2010;141:147-150
21. Bang CN, Gislason G, Kober L. et al. Statins reduce risk of new-onset AF after first-time myocardial infarction - A nationwide cohort study. European Heart Journal 32: 625. Eur J Prev Cardiol. 2012 [Epub ahead of print]
22. Rahimi K, Emberson J, McGale P. et al. Effect of statins on atrial fibrillation: collaborative meta-analysis of published and unpublished evidence from randomised controlled trials. BMJ. 2011;342:d1250
23. Miceli A, Fino C, Fiorani B. et al. Effects of Preoperative Statin Treatment on the Incidence of Postoperative Atrial Fibrillation in Patients Undergoing Coronary Artery Bypass Grafting. Ann Thorac Surg. 2009;87:1853-8
24. Adabag AS, Nelson DB, Bloomfield HE. Effects of statin therapy on preventing atrial fibrillation in coronary disease and heart failure. Am Heart J. 2007;154:1140-1145
25. Davidenkova EF, Shafron MG. Myeloperoxidase of neutrophils and its possible role in lipid peroxidation processes in arteriosclerosis. Klin Med (Mosk). 1989;67:56- 58
26. Malle E, Marsche G, Panzenboeck U. et al. Myeloperoxidase-mediated oxidation of high-density lipoproteins: Fingerprints of newly recognized potential proatherogenic lipoproteins. Arch Biochem Biophys. 2006;445:245- 255
27. Paoletti R, Gotto Jr AM, Hajjar DP. Inflammation in atherosclerosis and implications for therapy. Circulation. 2004;109:III20-6
28. Chung MK, Martin DO, Sprecher D. et al. C-reactive protein elevation in patients with atrial arrhythmias: Inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001;104:2886
29. Yao SY, Chu JM, Chen KP. et al. Inflammation in lone atrial fibrillation. Clin Cardiol. 2009;32:94-8
30. Das UN. Essential fatty acids as possible mediators of the actions of statins. Prostaglandins Leukot Essen Fatty Acids. 2001;65:37- 40
31. Adam O, Neuberger HR, Böhm M. et al. Prevention of Atrial Fibrillation With 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase Inhibitors. Circulation. 2008;118:1285-1293
32. Reilly SN, Jayaram R, Nahar K. et al. Atrial sources of reactive oxygen species vary with the duration and substrate of atrial fibrillation: implications for the antiarrhythmic effect of statins. Circulation. 2011;124:1107-17
Author contact
![]() Corresponding author: Yun-qing Chen, MD, Ph.D., Department of Cardiology, The Second Affiliated Hospital, Chongqing Medical University, No.76, Lingjiang Rd., Yuzhong District, Chongqing, P. R. China, 400010. E-mail: chenyunqing.88com
Corresponding author: Yun-qing Chen, MD, Ph.D., Department of Cardiology, The Second Affiliated Hospital, Chongqing Medical University, No.76, Lingjiang Rd., Yuzhong District, Chongqing, P. R. China, 400010. E-mail: chenyunqing.88com

 Global reach, higher impact
Global reach, higher impact