Impact Factor
ISSN: 1449-1907
Int J Med Sci 2011; 8(8):659-666. doi:10.7150/ijms.8.659 This issue Cite
Research Paper
Repercussions of Surgically Assisted Maxillary Expansion on Nose Width and Position of Septum and Inferior Nasal Conchae
1. Department of Oral and Maxillofacial Surgery, University of Pernambuco, Recife, Brazil
2. University of Pernambuco, Recife, Brazil
3. Department of Orthodontics, University of Pernambuco, Recife, Brazil
4. Department of Orthodontics/Department of Pediatric Dentistry, University of Pernambuco, Recife, Brazil
5. Department of Oral Medicine, University of Pernambuco, Recife, Brazil
Received 2011-6-3; Accepted 2011-7-27; Published 2011-10-21
Abstract
The aim of the present study was to assess the clinical and radiographic repercussions of surgically assisted maxillary expansion on the septum, nasal cavity and nasal conchae. The sample was made up of 15 patients with skeletal maturity (9 females and 6 males between 16 and 45 years of age) and maxillary transverse deficiency. Assessments were performed through anterior rhinoscopy and frontal cephalometric radiographs on three occasions: (T0) preoperative period, (T1) locking of the expander and (T2) six months following the locking procedure. An increase was observed in the basal portion of the pyriform aperture and distances between the lateral wall of the basal portion of the pyriform aperture and the septum. The radiographic exam revealed that the nasal septum did not undergo any statistically significant change in its position. Moreover, no significant changes in the position of the nasal septum or nasal conchae were detected throughout the three evaluation times. The results suggest that surgically assisted maxillary expansion is capable of widening the basal portion of the pyriform aperture, with little repercussion on the anterior position of the nasal septum and inferior nasal conchae.
Keywords: repercussions, septum, nasal cavity, nasal conchae, surgically assisted maxillary expansion
INTRODUCTION
Transverse maxillo-mandibular discrepancy is an important component of many skeletal malocclusions. Surgically assisted maxillary expansion is the procedure of choice in the treatment of transverse maxillary deformities in adults.5 This procedure is also indicated for patients who have undergone unsuccessful rapid orthopedic expansion, those with accentuated horizontal bone loss, those with cleft palate and transverse maxillary deformity and those with nasal stenosis.3,6,9 The objective of this procedure is to separate the sutures that impede palatine disjunction through modified Le Fort I osteotomy techniques involving the canine buttress, zygomatic buttress, pterygomaxillary sutures and median palatine suture.7 However, maxilla is related to ten bones of the viscerocranium in the central portion of the face and the surgical expansion may affect several associated anatomic structures, such as the mandible, temporomandibular joint, nasal cavity and septum.4,8
Studies in the literature have assessed the position of the septum following Le Fort I osteotomy, but few have related maxillary expansion to the nasal septum. The aim of the present study was to assess the position of the nasal septum, width of the nasal cavity and possible changes in the nasal conchae following surgically assisted maxillary expansion.
MATERIALS AND METHODS
The sample was made up of 15 patients with skeletal maturity (9 females and 6 males between 1 6 and 45 years of age) and maxillary transverse deficiency. No patients had any systemic disorders or past history of orthognathic surgery. The patients were submitted to surgically assisted maxillary expansion (SAME) and assessed with regard to the repercussions of this procedure on the nasal cavity and position of the nasal septum.
Assessment instruments
The patients were evaluated on three separate occasions for the determination of possible changes in the nasal cavity and position of the nasal septum: Time Zero (T0) - prior to treatment; Time 1 (T1) - during locking of expander 14 to 18 days following surgery; and Time 2 (T2) - at least six months following the locking of the expander. Table 1 displays the assessment scheme at each time. Tables 2 and 3 display the results obtained. The rhinological assessments were performed by a single examiner using the same protocol in all phases of the study. The radiographic assessments were performed by a specialist in dental radiology using an x-ray view box and digital caliper.
Sample evaluation scheme
| Data collection | Month | Sample |
|---|---|---|
| T0 | 1 | clinical assessment + radiographic exam + rhinoscopy |
| T1 | 2 | radiographic exam + rhinoscopy |
| T2 | 6 | clinical assessment + radiographic exam + rhinoscopy |
Methods used for assessment of patients at each evaluation time
Radiographic assessment of nose width at three evaluation times (T0, T1 and T2)
| PREOPERATIVE (T0) | LOCKING (T1) | POSTOPERATIVE (T2) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pat. | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) |
| 1 | 17.60 | 17.60 | 35.20 | 18.00 | 18.80 | 36.80 | 17.20 | 17.30 | 34.50 |
| 2 | 17.40 | 15.40 | 32.80 | 17.00 | 15.80 | 32.80 | 18.30 | 15.50 | 33.80 |
| 3 | 17.30 | 17.40 | 34.70 | 16.90 | 17.80 | 34.70 | 18.20 | 18.90 | 37.10 |
| 4 | 14.50 | 16.30 | 30.80 | 15.00 | 16.50 | 31.50 | 15.30 | 16.50 | 31.80 |
| 5 | 16.10 | 15.50 | 31.60 | 16.50 | 15.50 | 32.00 | 16.40 | 16.80 | 33.20 |
| 6 | 17.60 | 18.60 | 36.20 | 13.50 | 13.40 | 26.90 | 16.90 | 15.70 | 32.60 |
| 7 | 16.90 | 17.50 | 34.40 | 17.20 | 18.10 | 35.30 | 16.80 | 17.60 | 34.40 |
| 8 | 18.80 | 18.30 | 37.10 | 19.30 | 18.70 | 38.00 | 20.15 | 19.17 | 39.32 |
| 9 | 16.82 | 16.02 | 32.84 | 18.48 | 16.98 | 35.46 | 17.55 | 17.26 | 34.81 |
| 10 | 12.60 | 12.70 | 25.30 | 16.30 | 15.40 | 31.70 | 16.80 | 14.10 | 30.90 |
| 11 | 17.10 | 15.00 | 32.10 | 15.40 | 16.00 | 31.40 | 15.90 | 15.90 | 31.80 |
| 12 | 15.75 | 15.40 | 31.15 | 16.60 | 15.63 | 32.23 | 15.55 | 15.65 | 31.20 |
| 13 | 18.81 | 18.01 | 36.82 | 19.48 | 19.08 | 38.56 | 19.63 | 19.33 | 38.96 |
| 14 | 18.00 | 18.40 | 36.40 | 14.80 | 15.90 | 30.70 | 15.60 | 16.40 | 32.00 |
| 15 | 12.90 | 13.10 | 26.00 | 13.40 | 13.90 | 27.30 | 13.50 | 14.30 | 27.80 |
Point LP-S (R) and LP-S (L) respectively represent distances from lateral portion of the pyriform aperture to nasal septum on right and left sides
Radiographic assessment of position of nasal septum
| PREOPERATIVE (T0) | LOCKING (T1) | POSTOPERATIVE (T2) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pat. | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) | LP-S width (R) | LP-S width (L) | Nose width (NC-NC) |
| 1 | 0.50 | 0.50 | 35.20 | 0.49 | 0.51 | 36.80 | 0.50 | 0.50 | 34.50 |
| 2 | 0.53 | 0.47 | 32.80 | 0.52 | 0.48 | 32.80 | 0.54 | 0.46 | 33.80 |
| 3 | 0.50 | 0.50 | 34.70 | 0.49 | 0.51 | 34.70 | 0.49 | 0.51 | 37.10 |
| 4 | 0.47 | 0.53 | 30.80 | 0.48 | 0.52 | 31.50 | 0.48 | 0.52 | 31.80 |
| 5 | 0.51 | 0.49 | 31.60 | 0.52 | 0.48 | 32.00 | 0.49 | 0.51 | 33.20 |
| 6 | 0.49 | 0.51 | 36.20 | 0.53 | 0.47 | 26.90 | 0.52 | 0.48 | 32.60 |
| 7 | 0.49 | 0.51 | 34.40 | 0.48 | 0.52 | 35.30 | 0.49 | 0.51 | 34.40 |
| 8 | 0.51 | 0.49 | 37.10 | 0.51 | 0.49 | 38.00 | 0.52 | 0.48 | 39.32 |
| 9 | 0.52 | 0.48 | 32.84 | 0.52 | 0.48 | 35.46 | 0.50 | 0.50 | 34.81 |
| 10 | 0.50 | 0.50 | 25.30 | 0.51 | 0.49 | 31.70 | 0.54 | 0.46 | 30.90 |
| 11 | 0.53 | 0.47 | 32.10 | 0.49 | 0.51 | 31.40 | 0.50 | 0.50 | 31.80 |
| 12 | 0.51 | 0.49 | 31.15 | 0.52 | 0.48 | 32.23 | 0.50 | 0.50 | 31.20 |
| 13 | 0.51 | 0.49 | 36.82 | 0.51 | 0.49 | 38.56 | 0.50 | 0.50 | 38.96 |
| 14 | 0.49 | 0.51 | 36.40 | 0.48 | 0.52 | 30.70 | 0.49 | 0.51 | 32.00 |
| 15 | 0.50 | 0.50 | 26.00 | 0.49 | 0.51 | 27.30 | 0.49 | 0.51 | 27.80 |
Point LP-S (R) and LP-S (L) respectively represent percentage quantification (%) of distance from lateral portion of the pyriform aperture to nasal septum on right and left sides
Radiographic assessment of nose width at three evaluation times
| Variable | Phase | p-value | ||
|---|---|---|---|---|
| Preoperative (T0) Mean ± SD (1) | Locking (T1) Mean ± SD | Postoperative (T2) Mean ± SD | ||
| LP-S right | 16.55 ± 1.89 | 16.52 ± 1.87 | 16.92 ± 1.71 | p (2) = 0.489 |
| LP-S left | 16.35 ± 1.85 | 16.50 ± 1.73 | 16.69 ± 1.61 | p (2) = 0.557 |
| NC-NC | 32.90 ± 3.61 | 32.02 ± 3.46 | 33.61 ± 3.09 | p (2) = 0.316 |
| p-value | p (3) = 0.469 | p (3) = 0.923 | p (3) = 0.489 | |
(1) SD = standard deviation
(2) F test (ANOVA) with repeated measurements for comparison of each variable between evaluation times
(3) Paired Student's t-test for comparison between right and left side in each phase
Radiographic assessment of position of nasal septum at three evaluation times
| Variable | Phase | p-value | ||
|---|---|---|---|---|
| Preoperative (T0) Mean ± SD (1) | Locking (T1) Mean ± SD | Postoperative (T2) Mean ± SD | ||
| P-NS-L-LP-S-right | 0.50 ± 0.02 | 0.50 ± 0.02 | 0.50 ± 0.02 | p (2) = 0.954 |
| P-NS-L-LP-S-left | 0.50 ± 0.02 | 0.50 ± 0.02 | 0.50 ± 0.02 | p (2) = 0.954 |
(1) SD = standard deviation
(2) F test (ANOVA) with repeated measurements for comparison of each variable between evaluation times
Rhinological assessment
The physical exam of the nasal cavity (anterior rhinoscopy), including the clinical evaluation of the position of the nasal septum, was performed by an otolaryngologist from the Pedro II Hospital- Pernambuco (Brazil). Anterior rhinoscopy was performed following the method described by Meirelles and Atherrino.12 For such, the nasal speculum was inserted into the nasal vestibule with the blades closed and the lower portion slightly lateralized. The blades were then gently opened to obtain a view of the internal structures of the nasal fossa, such as the septum, conchae, floor, valve and, in some cases, the middle meatus and middle concha. The wing of the nose was secured with the index finger to impede abrupt movements of the patient's head that could cause intra-nasal trauma. Pressure on the lateral wall, inferior concha and anterior wall of the septum was avoided in order to prevent the occurrence of pain and bleeding.
Radiographic assessment
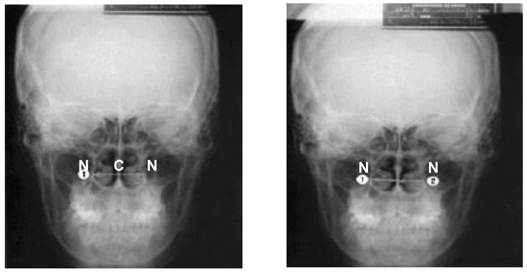
The radiographs were taken in the same radiology clinic following the same protocol and assessed by a single specialist in dental radiology. The frontal cephalometric radiograph was used for the analysis of the treatment of transverse deformity and associated structures.4 The radiograph was positioned on the x-ray viewer box and the measurements were taken using a digital caliper (Starret®). Nose width and position of the nasal septum in relation to the left and right lateral walls of the pyriform aperture were determined. The measurements were taken twice during each evaluation time in order to confirm the data. The NC and CN cephalometric points, which represent the distances from the base of the pyriform aperture to the nasal septum on both sides, were used to determine nose width. The sum of these two measurements represents the transverse diameter of the nose (Fig 1). As linear measurements alone would not allow determining whether the movement following SAME was of the lateral wall of the pyriform aperture or the nasal septum itself, the position of the septum was also analyzed through the percentage quantification of the distance from the septum to the lateral wall of the pyriform aperture (cephalometric point N).8
Surgical procedure
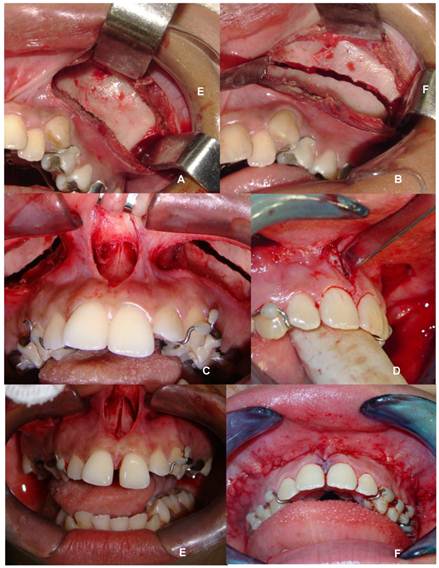
The surgical procedure was performed under anesthesia in a hospital setting by the same surgical team following the technique described by Bays and Greco.3 All patients used the tooth-supported Hyrax expander. The surgical technique consisted of osteotomy of the lateral wall of the maxilla associated to that of the median palatine suture. A full-thickness muco-periosteal flap was confected through a horizontal incision in the fundus of the vestibular sulcus from canine to molar, bilaterally, exposing the entire length of the lateral wall of the maxilla. A second surgical access was performed in the anterior region bordering the insertion of the upper labial frenulum, exposing the anterior region of the median palatine suture and anterior nasal spine. The osteotomy line extended from the lateral wall of the pyriform aperture to the region of the zygomaticomaxillary buttress, bilaterally. In the anterior region, osteotomy of the median palatine suture and alveolar ridge between the incisors was performed with the aid of chisels (Fig 2). Bone separation was verified through the activation of the expander, with the observation of clinical signs of ischemia of the incisive papilla and the presence of diastema between the incisors. During the operation, the patient received an expansion of 1.0 mm (4/4 turns).
On the seventh day of the postoperative period, the patient returned for follow up. The activation of the expander was initiated, with two daily 2/4 turns. Following the transverse correction of the maxilla, the expander was locked for a four-month containment period, followed by the subsequent installment of a fixed appliance.
Scheme for radiographic measurements of nasal cavity and septum8
(A) - Incision in fundus of vestibular sulcus between canine and molar; (B) Osteotomy of lateral wall of maxilla from pyriform aperture to maxillary tuber; (C) Access to median palatine suture; (D) Positioning of osteotome for separation of median palatine suture; (E) Osteotomy of median palatine suture and diastema between central incisors (clinical sign of effective expansion); (F) Synthesis (ROCHA, 2008)
Statistical methods
Data analysis involved the determination of mean and standard deviation values. The paired Student's t-test and the F test (ANOVA) for repeated measurements with the Greenhouse-Geisser correction were used. The level of significance was set at 5.0%. The Statistical Package for the Social Sciences (SPSS, version 15) was used for the data entry and statistical calculations.
RESULTS
Among the 15 patients analyzed, nine (60%) were female and six (40%) were male. Mean age was 23.8 years, ranging from 16 to 45 years. The main reasons that led the patients to seek treatment were problems with the occlusion (66.66%), pain and esthetics (17.64%) and breathing problems (11.76%).
Following the initial rhinological evaluation, no substantial alterations were diagnosed that would indicate septoplasty or turbinectomy prior to maxillary expansion. The preoperative rhinoscopic exam revealed that five patients (33.33%) had a deviated septum and four (26.66%) exhibited hypertrophy of the nasal conchae. However, none of these patients exhibited a change in these conditions on the assessment performed after the surgical intervention.
Table 4 displays the mean and standard deviation values of the measurements at each evaluation time on the right and left sides and the width of the nasal cavity. No statistically differences were detected in these variables between sides or between evaluation periods (p > 0.05). Table 5 displays the mean position values. All mean values were 0.50 in each phase, with no statistically significant differences between phases (p > 0.05).
DISCUSSION
One of the earliest descriptions of the treatment of maxillary atresia through surgical procedures in the medical-dental literature is from Angle in 1860. Surgically assisted maxillary expansion (SAME) is a widely used procedure for the treatment of transverse maxillary deformities in individuals who have reached skeletal maturity. The aim of the treatment of such conditions is to increase the transverse dimension of the maxilla through osteotomy of the skeletal sutures and subsequent bone distraction of the maxillae. In individuals with skeletal maturity, SAME has demonstrated good results and its effects are also seen in the nasal cavity, with an improvement in breathing due to the increase in nasal volume.13
The effects of SAME on the nasal cavity and breathing pattern began to be studied around 1886 and are currently the object of numerous studies and divergent opinions. Anatomically, there is an increase in the width of the nasal cavity immediately following maxillary expansion, particularly in the nasal floor near the median palatine suture.9 The osteocartilaginous nasal septum is located in the median portion and the nasal cavity and is deviated in the preoperative period in approximately 20% of cases, with the majority of patients assymptomatic.21 When a patient has respiratory difficulties related to a deviated septum, special care must be given to this cause of nasal obstruction, as it is generally associated to maxillary atresia. According to Wollens et al., SAME can either improve the position of the nasal septum or aggravate a preexisting deviation, thereby suggesting awaiting the achievement of the expansion and reassessing the need for the surgical correction of the deviated septum.21
Some patients who require orthognathic surgery have a coexisting nasal deformity, which may be of functional or esthetic significance. In such cases, it is more convenient for both the patient and professional team to correct the deformity concomitantly to the orthognathic surgery.7 With the joint work of the maxillofacial surgeon and orolaryngologist in cases in which SAME is scheduled and the patient has also impaired nasal function due to a deformed septum, both procedures - maxillary osteotomy and septoplasty - can be performed during the same surgical act.13
Although some authors have found no changes in the nasal septum, the anatomic description of this structure reveals that it may interfere in the expansion of the maxilla or move together with it during expansion.11 According to Lanigan and Mintz, there are numerous surgical techniques described in the literature for maxillary expansion, the most invasive of which are reserved for patients with large discrepancies and/or a more advanced age.11 However, these techniques do not establish the total osteotomy of the nasal septum, thereby favoring changes in its position during expansion, which could lead to deviation.
Osteotomy of the nasal septum is generally defended to prevent the deviation of the septum during the separation of the maxillary bones.2 However, studies assessing this movement through radiographs and tomograms have not found statistically significant differences between cases in which osteotomy was performed and those in which this procedure was not performed.18 Both theories subjectively suggest possible alterations in the position of the nasal septum following SAME. However, none of the studies consulted assesses clinical and radiographic alterations in the position of the nasal septum following the procedure. Thus, the present study offers a discussion regarding the clinical and radiographic effects of SAME on the position of the nasal septum, investigating the possibility of the fixation of the nasal septum to one of the maxillae, thereby triggering a deviation following bone distraction, as the surgical technique employed does not involve osteotomy of the septum.
During the oral examination, 100% of the 15 patients evaluated had bilateral posterior crossbite and 80% had a high-arched palate. Andrade et al. assessed the occurrence of nasal obstruction and septum deformity in adult patients with posterior crossbite.1 For such, the authors carried out a rhinological assessment using nasal fibroscopy on 30 adult patients with posterior crossbite and indicated for orthodontic-surgical treatment (SAME). A total of 56.7% of the patients reported nasal obstruction, whereas the other 43.3% had no breathing complaints. The authors concluded that adult patients with skeletal posterior crossbite do not necessarily have nasal obstruction.
In the present study, anterior rhinoscopy revealed a deviated septum in five (33.33%) patients in the preoperative period. This deviation remained following the surgical intervention for maxillary atresia and the later clinical assessments revealed no changes. In the study by Andrade et al., all of the 30 patients with an indication for orthodontic-surgical treatment exhibited some degree of septum deformity prior to the procedure.1 The difference in percentage values regarding the prevalence of preoperative deviated septum between the two studies may be related to a conditioned sample or the type of exam used, which was nasal fibroscopy in the Andrade et al. study. This exam provides a more faithful assessment of the position of the nasal septum throughout its anteroposterior extension. In the present study, anterior rhinoscopy was performed, as no equipment was available for the nasal fibroscopic exam. However, there was no loss in the quality of the diagnosis of the anterior deviation of the nasal septum, as the clinical exam together with the radiographic exam is adequate for this purpose.
Gonçalves et al. assessed the behavior of the nasal septum with regard to SAME procedures using anteroposterior cephalometric radiographs and total occlusal radiographs of the maxilla.8 The sample was made up of 16 patients and the surgical technique employed was subtotal Le Fort I osteotomy. Frontal cephalometry was used in the study, as this standard radiographic exam is used for the assessment of maxillary expansion and allows adequate visualization of the anterior portion of the nasal septum. The radiographs were taken in the preoperative period (initial) and in the mediate postoperative period or at the end of expansion. In the present study, the radiographic assessment of the position of the nasal septum following SAME was also performed with frontal cephalometric radiographs. However, the evaluations were carried out on three occasions: the preoperative period (T0); at the locking of the expander with maximal maxillary expansion (T1); and six months after the procedure (T2). This allowed radiographic follow up of the position of the septum throughout all steps of the procedure. The nasal septum did not undergo any significant radiographic change in its position following SAME at either postoperative evaluation time. These data are in agreement with those reported in the study by Gonçalves et al., who also found no change in the position of the nasal septum following SAME.8
There are three conchae (superior, middle and inferior) in the interior of the lateral walls of the nasal cavity, the main function of which is to hinder the passage of air to the rest of the airways, causing a change from laminar flow to a turbinate flow, which makes the air strike the walls of the nasal cavity and the conchae more, placing the air into greater contact with the moisture of the mucosa. In the process, the air is also heated through contact with the conchae, which are highly vascularized and therefore have a high temperature. This phenomenon results in the transformation of cold dry outer air into warm moist air for the lungs, which is essential to breathing. In orthognathic surgery, the nasal conchae are studied mainly in the upper repositioning in the maxilla. A number of authors defend their removal in order to avoid the contact of this structure with the floor of the nasal fossa and possible recurring nasal obstruction.7
Observing its relation with the nasal septum, a deviated septum generally leads to hypertrophy of the conchae. With the correction of the deviation, the conchae tend to return to their normal physiological form. In cases in which there is very severe hypertrophy or calcification of the hypertrophic concha, the return to physiological function does not occur in an adequate fashion and the partial resection of the conchae is necessary. Among the three different conchae, the inferior concha exerts the greatest influence over nasal obstructions related to the hypertrophy of these structures. Hypertrophy of the inferior nasal conchae was found in four patients (26.66%) in the present study, all of whom had a deviated septum. However, none of these patients had an indication for surgery prior to maxillary expansion and there was no change in the clinical condition during the postoperative follow up. A clinical assessment in such patients is of fundamental importance, as a diagnosis of concha hypertrophy may be relative due to a narrow nasal cavity stemming from a transverse maxillary deformity.
Among the 15 patients in the sample, only one reported having a nasal-breathing pattern. According to Vidotti and Trindade, this effect is of particular importance because nasal obstruction can lead to atresia of the maxillary arch and maxillary atresia can determine a decrease in the width of the nasal cavity, which theoretically compromises nasal permeability (the passage of air through the nasal cavity), leading to a mouth-breathing pattern.19 A number of studies have reported an improvement in nasal breathing stemming from the gain in nasal cavity volume and reduction in nasal aerial resistance following the oto-surgical treatment of maxillary atresia.14 Ramires, Maia and Barone carried out a literature review to assess alterations in the nasal cavity and breathing pattern following maxillary expansion involving experimental studies, including those that employed SAME and excluding those that employed segmental osteotomy maxillary expansion for the treatment of maxillary atresia.13 The authors concluded that both techniques lead to dentofacial alterations, especially in the nasal cavity, causing an increase in nose width, which can lead to a reduction in nasal aerial resistance.
SAME proved to have discreet clinical and radiographic effects on the position of the nasal septum. Among the patients with hypertrophy of the nasal conchae in the preoperative evaluation, no changes in the clinical condition were observed during the control evaluations, thereby suggesting that SAME does not have repercussions on the nasal conchae.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Andrade AIA, Russo LCP, Lima MLLT, Oliveira LCS. Septal deformity evaluation by nasofibroscopy in adult patients with transverse maxillary deficiency. Rev Bras Otorrinolaringol. 2002;68(5):639-44
2. Araújo A. Cirurgia Ortognática. Santos: São Paulo. 1999
3. Bays RA, Greco JM. Surgically assisted rapid palatal expansion: na outpatient technique with long-term stability. J. Oral Maxillofac Surg. 1992:110-113
4. Betts NJ. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthod Orthognath Surg, Chigago. 1995;10(2):75-96
5. Capelozza Filho L, Mazzottini R, Neto JC, Silva Filho OG. Expansão rápida da maxila cirurgicamente assistida. Ortodontia. 1994;27(1):21-29
6. Capelozza filho L, Silva filho OG. Expansão rápida da maxila: considerações e aplicações clínicas. Ortodontia: bases para a iniciação. 4ed. São Paulo: Artes médicas. 1999
7. Epker BN, Wolford LM. Dentofacial Deformities: surgical-orthodontic correction. St. Louis: Ed Mosby. 1980
8. Gonçalves ES, Assis DSFR, Capelozza ALA, Alvares LC. Estudo radiográfico digital indireto do efeito da expansão de maxila cirurgicamente assistida sobre o septo nasal. Revista Dental Press Ortodon Ortop Facial, Maringá. 2007;2(5):85-91
9. Hass AJ. Rapid expansion of the maxillary dental arch and nasal cavity opening the midpalatal suture. Angle Orthod. 1961;3:73-90
10. Jacobs JD, Bell WH, Williams CE, Kennedy JW3rd. Control of the transverse dimension with surgery and orthodontics. Am J Orthod. 1980;77:284-306
11. Lanigan DT, Mintz SM. Complications of surgically assisted rapid palatal expansion: review of the literature and report of a case. J. Oral Maxillofac. Surg. 2002;60:104-110
12. Meirelles RC, Atherino CCT. Semiologia em Otorrinolaringologia - manual para clínicos e pediatras. São Paulo: Brasil Fundo Editorial Byk. 2004:1-47
13. Ramires T, Maia RA, Barone JR. Alterações da cavidade nasal e do padrão respiratório após expansão rápida da maxila. Rev. Bras. Otorrinolaringol. 2008;74(5):763-769
14. Ribeiro Junior PD, Gonçales ES, Souza PCU, Nary Filho H, Luz JGC. Avaliação clínica dos procedimentos de expansão cirurgicamente assistida da maxila. Rev Dental Press Ortodon Ortop Facial. 2006;11(1):44-59
15. Rocha NS, Oliveira DM, Laureano Filho JR, Vasconcellos RJH, Caubi AF. Discrepância transversal da maxila: tratamento ortodôntico-cirúrgico. Braz J Oral Maxillofac Surg. 2005;5(2):55-60
16. Rocha NS. Avaliação do efeito da expansão cirugicamente assistida da maxila sobre a função auditiva. Camaragibe; [Dissertação de Mestrado em Cirurgia Buco-Maxilo-Facial]. Faculade de Odontologia da Universidade de Pernambuco. 2008
17. Suri L, Taneja P. Surgically assisted rapid palatal expansion: A literature review. Am J Orthod Dentofacial Orthop. 2008;133:290-302
18. Taspinar F, Üçüncü H, Bishara SE. Rapid maxillary expansion and conductive hearing loss. Angle Orthod. 2003;73(6):669-673
19. Vidotti BA, Trindade EK. Os efeitos da expansão rápida da maxila sobre a permeabilidade nasal avaliados por rinomanometria e rinometria acústica. R Dental Press Ortodon Ortop Facial. 2008;13(6):59-65
20. Villano A, Grampi B, Fiorntini R, Gandini P. Correlations between rapid maxillary expansion (RME) and auditory apparatus. The Angle Orthodontist. 2006;76(5):752-758
21. Wollens AG, Goffart Y, Lismind P, Limme M. Expansion thérapeutic du maxillaire. Amsterdan: Rev Belge Méd Dent. 1994:4
Author contact
![]() Corresponding author: Liana P. Carvalho Studart, lianapcarvalhocom
Corresponding author: Liana P. Carvalho Studart, lianapcarvalhocom

 Global reach, higher impact
Global reach, higher impact