3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2011; 8(1):1-8. doi:10.7150/ijms.8.1 This issue Cite
Research Paper
6-Month Results of Transdiscal Biacuplasty on Patients with Discogenic Low Back Pain: Preliminary Findings
1. Pain Management Center, Department of Anesthesiology, Dicle University, Diyarbakir, TURKEY
2. Department of Anesthesiology, Dicle University, Diyarbakir, TURKEY
3. Department of Anesthesiology, Diyarbakir Training and Research Hospital, Diyarbakir, TURKEY
4. Diyarbakır Vocational Higher School, Department of Technique, Dicle University, Diyarbakir, TURKEY
Received 2010-10-21; Accepted 2010-12-9; Published 2010-12-14
Abstract
Study Design: Prospective observational study.
Objective: Our aim is to investigate the efficacy and safety of TransDiscal Biacuplasty.
Summary of Background Data: Chronic discogenic pain is one of the leading causes of low back pain; however, the condition is not helped by most non-invasive methods. The results of major surgical operations for these patients are unsatisfactory. Recently, attention has shifted to disk heating methods for treatment. TransDiscal Biacuplasty is one of the minimally invasive treatment methods. The method was developed as an alternative to spinal surgical practices and Intradiscal Electrothermal Therapy for treatment of patients with chronic discogenic pain.
Methods: The candidates for this study were patients with chronic discogenic pain that did not respond to conservative treatment. The main criteria for inclusion were: the existence of axial low back pain present for 6 months; disc degeneration or internal disc disruption at a minimum of one level, and maximum of two levels, in MR imaging; and positive discography. Physical function was assessed using the Oswestry Disability Index when measuring the pain with VAS. Patient satisfaction was evaluated using a 4-grade scale. Follow-ups were made 1, 3, and 6 months after treatment.
Results: 15 patients were treated at one or two levels. The mean patient age was 43.1±9.2 years. We found the mean symptom duration to be 40.5±45.7 months. At the sixth month, 57.1% of patients reported a 50% or more reduction in pain, while 78.6% of patients reported a reduction of at least two points in their VAS values. In the final check, 78.6% of patients reported a 10-point improvement in their Oswestry Disability scores compared to the initial values. No complications were observed in any of the patients.
Conclusions: TransDiscal Biacuplasty is an effective and safe method.
Keywords: discogenic pain, low back pain, transdiscal biacuplasty, intradiscal electrothermal therapy, cool radiofrequency
INTRODUCTION
A large percentage of low back pain results in a high rate of morbidity. While an important amount of labor lost due to this pain can be relieved by non-invasive conservative treatment, unfortunately, about 5% of this pain becomes chronic. This pain continues to be the underlying cause of severe pain and functional disorder.1 Almost 90% of health care expenditures aimed at the treatment of low back pain go to help this patient group with severe pain.2 Although there are many sources of pain in the low back region, intervertebral discs are one of the most important sources of this pain. It believes that Internal Disc Disruption (IDD) is the cause of 40% of chronic, persistent, low back pain of unknown origin.3
For most lumbago patients with marked with IDD evidence in their imaging methods, and pain that has lasted for over three months, non-invasive conservative treatment methods, such as medical treatment and physical therapy cannot be successful alone.1,4 In these patients, spinal fusion and artificial disk replacement surgeries using open surgical methods do not yield satisfactory results as well.5-7 Intradiscal Electrothermal Therapy (IDET) is one of the minimally invasive treatment methods. The method was developed as an alternative to spinal surgical practices for treatment of patients with chronic discogenic pain.8-11 Using this technique, the thermal therapy targets the annulus of the disc using a navigable intradiscal catheter at a temperature range that both modulates the collagen properties of the disc and destroys the nociceptive nerve endings.6 Because intradiscal electrothermal therapy (IDET), considered as an intermediary step between conservative treatments and major surgical interventions, produced varying results in the pain reduction and functional improvement, and has been shown to benefit a small group of properly selected patients, the use of this method is limited.12-14 Also, technical difficulties in its application are other disadvantage of this method.
TransDiscal Biacuplasty (TDB) is one of the minimally invasive treatment methods recently developed for the treatment of chronic discogenic pain.15 It has been argued that wider and safer thermal lesioning was done at posterior annulus with this method using bipolar cooled radiofrequency energy.16,17 In addition, this method is much easier to apply than IDET. This advantage will reduce the potential risk of application-related complications. The initial study results of the effectiveness of TDB, a new practice, are promising.12,15
In this study, we aim to prospectively explore the long-term effectiveness and security of TDB. We want to provide information about the effectiveness and safeness of TDB by publishing early-period outcomes of our currently on-going study.
MATERIALS AND METHODS
Study Design and Setting
This study is being conducted with patients on an outpatient basis method at the pain center of a university hospital, following Institutional Review Board approval. Recruitment of patients for treatment with TDB started in April 2009. The study was planned as a prospective, observational, non-controlled and non-randomized research. We obtained written consent from all patients who participated after they were informed both verbally and in writing about the procedure and the study.
Follow-up period; patients were independently evaluated by a non-participating doctor at baseline and at 1, 3 and 6 months after the procedure.
Participants
Inclusion criteria were: 1) presence of a predominant axial chronic low back pain lasting for a minimum of 6 months; 2) no response to detailed non-invasive conservative treatment methods like non-steroidal anti-inflammatory drugs, physical therapy and fluoroscopically guided epidural steroid injection; 3) low back pain more severe than leg pain and increased pain after sitting; 4) normal lower extremities in neurological examination; 5) disc degeneration or IDD findings at a minimum of one level, and maximum of two levels, in MR imaging (MRI); 6) finding of a disc height loss less than 50% in Anterior-Posterior (AP) and lateral plain radiography; and 7) demonstration of positive concordant pain of intensity >6/10 during provocative lumbar discography at 1 or 2 disc levels at low pressures (<50 psi) with negative control disc at one and preferably two adjacent levels.
Exclusion criteria were as follows: 1) more prominent radicular leg pain; 2) more than two disc degenerations or IDD findings on MRI; 3) an extruded or sequestered herniated nucleus pulposus; 4) presence of >%30 spinal canal stenosis evidenced by MRI or CT; 5) previous spinal surgical application for any reason at the level(s) to be treated; 6) spondylolisthesis in symptomatic level(s); 7) patients over sixty; 8) patients with psychiatric disorders; 9) pregnancy; and 10) presence of general contraindications to the application of any invasive intervention (such as bleeding diathesis, systemic infections or local infections in the field of intervention, known history of allergy to substances to be used).
Procedures
All applications were made with C-arm fluoroscopy under local anesthesia. Patients were taken into the operation room following application of antibiotics intravenously 2 hours before the intervention. All patients were taken to the fluoroscopy table in prone position following routine monitoring (containing pulsoximetry, TA and ECG). After the area to undergo intervention was cleaned with iodine antiseptic solution, it was covered in compliance with the rules of sterility. Sedation was not attempted in order not to mask potential complications. However, when necessary, 1-3 mg midazolam and/or 50-100 mcg fentanyl were intravenously administered. The symptomatic disk was reached in oblique position after cutaneous-subcutaneous anesthesia using lidocaine 1%. To facilitate the intervention, first both posterolateral parts of the disc were bilaterally accessed by 17 G introducer needle (Baylis Medical Inc., Montreal, Canada). Then, two radiofrequency (RF) probes (Baylis Medical Inc., Montreal, Canada) specially designed for cooled radiofrequency practice, wherein closed circuit sterile water circulates, were fitted into the disc after they were passed through the introducers. To ensure that the probe tip was at optimal depth in the posterior annulus, the location of the probe in the tissue was controlled in lateral and AP positions, with the radio opaque band at its tip taken as reference. TDB was applied with the software (Set Temperature = 45oC, Ramp Rate = 2.0oC/min, Time = 15 minutes) previously installed into the device by its producer. Continuous communication was maintained with the patient throughout the intervention to prevent complications. After completion of the intervention, needle penetration sites were bandaged, and the patient was kept on the table for 5 minutes. Then, the patients were transferred to the recovery room where they stayed for 4 hours. The patients were discharged with certain recommendations, and followed by a clinic physician and nurse only for early complications. They were recommended to wear lumbar braces for a period of 6 to 8 weeks after the intervention. The patients were allowed to walk, sit, and stand unlimitedly starting 24 hours after the operation. The patients were told that they could start doing light jobs 3 to 4 days after the procedure and were asked not to lift more than 4 kilograms for a period of 2 weeks. They were recommended to start gentle stretching exercises at their homes after 2 weeks.
Outcome measurements
Pain; was evaluated using 10 cm VAS score. In this scale, “0” described a condition with no pain, and “10” describes the worst pain imaginable.
Physical condition; was evaluated by Oswestry Disability Index (ODI). This is a questionnaire of a maximum of 50 points organized in 10 sections, with six options in each section. Higher scores indicate poorer physical condition. The scores made are translated into percentile scores to calculate the disability index.
Patient Satisfaction Scale (PSS); Patient satisfaction was evaluated based on a 4-grade scale: 1-poorly satisfied, 2-moderately satisfied, 3-fairly satisfied, and 4-extremely satisfied.
The patients' age, sex, duration of symptom, IDD or degeneration disc levels were also gathered for statistical analysis.
Statistical methods
All data were analyzed using the statistical package SPSS version 15.0 for Windows and Medcalc Version 10.3.0.0 for Windows. Repeated Measurements ANOVA parametric test for repeated measurements was used to evaluate the improvements in VAS and ODI scores both before and after the procedure. When the Repeated Measurements ANOVA test showed a statistical difference, we used a paired samples t-test with Bonferonni's correction to perform pairwise comparisons. Also, we used the Spearman correlation coefficients to study the effects of various factors on the outcomes. P < 0.05 was considered statistically significant in all analyses.
RESULTS
Demographic Characteristics
15 patients who completed their 6-month follow-up periods were studied. One of these patients was lost at the 6th month follow-up; therefore, a total of 14 patients completed their follow-ups. The mean age of patients in the study was (±SD) 43.1±9.2 years, 10 of them were female. 14 patients were treated at one level; one patient was treated at two levels. The L4-L5 and L5-S1 were the most frequently treated levels. The average symptom time of fifteen patients was calculated as (±SD) 40.5±45.7 months (Table 1).
Demographic characteristics
| AGE (years) | mean±SD | 43.1±9.2 |
| range | 25-60 | |
| SEX n (%) | women | 10 (66.7) |
| men | 5 (33.3) | |
| DURATION OF PAIN (months) | mean±SD | 40.5±45.7 |
| range | 12-168 | |
| TREATED LEVELS n (%) | L3-4 | 4 (25) |
| L4-5 | 6 (37.5) | |
| L5-S1 | 6 (37.5) | |
| NUMBER OF TREATED LEVELS | one | 14 |
| two | 1 |
SD, standard deviation.
Outcome Data
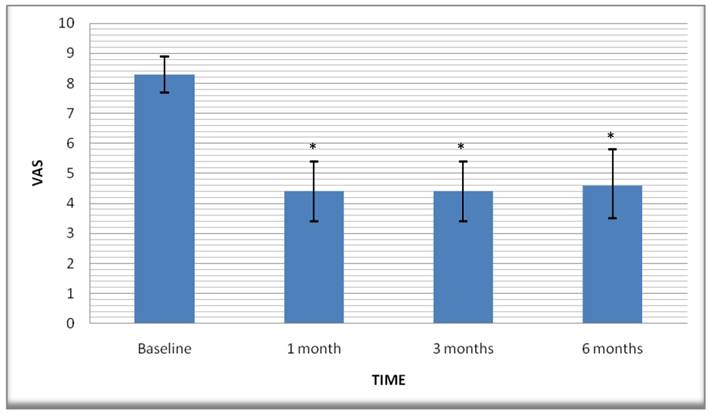
Pain relief; while the mean VAS score before the procedure was (±Std. Error) 8.3±0.3, it dropped to 4.4±0.5 in the 1st month. The 3rd and 6th month scores were 4.4±0.5 and 4.6±0.5 respectively (Figure 1). When the baseline VAS scores were compared to VAS scores at all follow-up periods, a statistically significant difference was found between them. However, no statistically significant difference was found between the follow-up periods (Table 2). Thus, we found a 43.4% decrease in the average VAS score compared to the initial values at the final follow-up. While 57.1% of patients reported a 50% or more increase in their pain at the 6th month check, 78.6% of patients reported a decrease of at least two points in their VAS scores.
Graphic showing decreases of the VAS pain scores over the time in patients. Values are shown as means (error bars: 95% CI for mean). VAS, Visual Analog Scale. *Statistically significant decrease.
Pair-wise comparisons of all-time VAS and ODI scores
| Mean Difference | Std. Error | P a | 95% CI a | |||
|---|---|---|---|---|---|---|
| VASBaseline | - | VAS1 month | 3.857 | 0.573 | 0.0001 | 2.077 to 5.637 |
| - | VAS3months | 3.929 | 0.606 | 0.0001 | 2.044 to 5.813 | |
| - | VAS6 months | 3.643 | 0.684 | 0.0008 | 1.517 to 5.769 | |
| VAS1month | - | VAS3 months | 0.0714 | 0.165 | 1.0000 | -0.440 to 0.583 |
| - | VAS6 months | -0.214 | 0.281 | 1.0000 | -1.087 to 0.658 | |
| VAS3months | - | VAS6 months | -0.286 | 0.194 | 0.9889 | -0.889 to 0.317 |
| ODIBaseline | - | ODI1 month | 17.571 | 2.674 | 0,0001 | 9.263 to 25.880 |
| - | ODI3 months | 17.643 | 2.781 | 0,0002 | 9.003 to 26.282 | |
| - | ODI6 months | 17.000 | 2.920 | 0,0004 | 7.927 to 26.073 | |
| ODI1 month | - | ODI3 months | 0.0714 | 0.624 | 1,0000 | -1.868 to 2.011 |
| - | ODI6 months | -0.571 | 1.015 | 1,0000 | -3.724 to 2.582 | |
| ODI3months | - | ODI6 months | -0.643 | 0.668 | 1,0000 | -2.718 to 1.433 |
aBonferroni corrected.
VAS, Visual Analog Scale; ODI, Oswestry Disability Index.
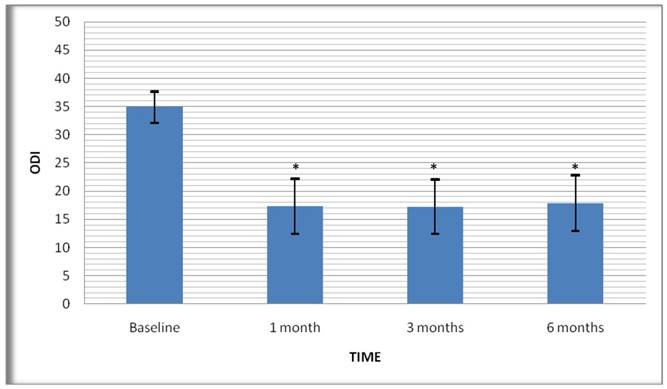
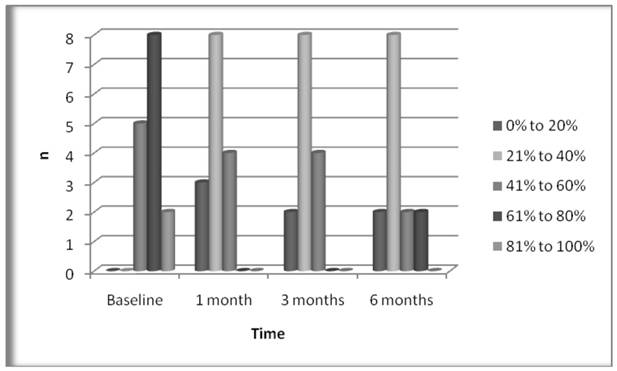
Physical recovery; the mean score of patients was (±Std.Error) 34.9±1.3 before the treatment according to the evaluation of physical recovery with a 50-grade ODI. While ODI scores were reduced to 17.3±2.3 at the first follow-up after the treatment, the 3rd and 6th month scores were 17.2±2.2 and 17.9±2.3 respectively (Figure 2). Comparison of baseline ODI scores and ODI scores at all follow-up periods showed statistically significant difference between them, and no statistically significant difference between the follow-up periods (Table 2). At the final follow-up, the rate of patients reporting a 10-point decrease in their ODI scores compared to the initial value was found as 78.6%. An examination of the Oswestry disability index showed five of the patients were in the 41-60% segment (severe disability, C), 8 and 2 of them, respectively, were in the 61-80% (disability, D) and 81-100% (bed-bound, E) disability segment before the treatment. There were no patients in the 0-20% (minimal disability, A) and 21-40% (moderate disability, B) segment. However, at the final follow-up, 10 of the patients were in the A and B segments. We had no patients in the E segment (Figure 3).
Graphic showing improvements of the ODI scores over the time in patients. Values are shown as means (error bars: 95% CI for mean). ODI, Oswestry Disability Index. *Statistically significant improvement.
Graphic showing disability indexes of the patients over the time. There are significant improvements in disability indexes at all follow-up periods.
Moreover, based on the results from the final follow-up, we studied the effects of various factors such as age, sex and duration of symptom on ODI, VAS and PSS scores. While a correlation (positive with ODI and VAS, and negative with PSS) was observed with the duration of symptom, no correlation was found with the other factors (Table 3). Furthermore, we found a positive correlation among themselves in the decreases in VAS and ODI scores in the 6th month compared to the baseline period (Table 4).
Effects of various factors on outcome at 6 month after treatment
| VAS | ODI | PSS | |||
|---|---|---|---|---|---|
| Spearman's rho | Sex | Correlation Coefficient | .113 | .145 | .000 |
| Sig. (2-tailed) | .700 | .621 | 1.000 | ||
| N | 14 | 14 | 14 | ||
| Duration of symptoms | Correlation Coefficient | .640* | .599* | -.588* | |
| Sig. (2-tailed) | .014 | .024 | .027 | ||
| N | 14 | 14 | 14 | ||
| Age | Correlation Coefficient | .264 | .345 | -.294 | |
| Sig. (2-tailed) | .362 | .227 | .308 | ||
| N | 14 | 14 | 14 | ||
* Correlation is significant at the 0.05 level (2-tailed).
VAS, Visual Analog Scale; ODI, Oswestry Disability Index; PSS, Patient Satisfactory Scale.
Correlations between the post-procedure changes in VAS and ODI scores
| VAS | ODI | |||
|---|---|---|---|---|
| Spearman's rho | VAS | Correlation Coefficient | 1.000 | .989** |
| Sig. (2-tailed) | . | .000 | ||
| N | 14 | 14 | ||
| ODI | Correlation Coefficient | .989** | 1.000 | |
| Sig. (2-tailed) | .000 | . | ||
| N | 14 | 14 | ||
**.Correlation is significant at the 0.01 level (2-tailed)
VAS, Visual Analog Scale; ODI, Oswestry Disability Index.
Patient satisfaction; satisfaction of patients were evaluated using a four-grade scale (where 1 shows least satisfaction and 4 shows highest satisfaction), 71.4% of patients said they were fairly or extremely satisfied at the final check (10 patients).
Safety; No major complications, such as nerve injuries, discitis, bleeding and hematoma were encountered during or after the application. The only two minor complications occurred. One was low back pain seen in all patients and lasting for one-two days, depending on the application. Another was vasovagal reaction that was only seen in one patient, and this patient was recovered with fluid support and trendelenburg positioning within 30 minutes.
DISCUSSION
Despite the presence of many biomechanical and neurological components that may cause low back pain, disc disease is one of its leading causes.18 Disc disease is a condition characterized by the destruction of collagens in annulus fibrosis.10 Destruction of collagens leads to posterior annular radial fissuring, delamination and disc degeneration. Although radial fissures are not attributes of degeneration, and although there are no correlations between degenerative changes and pain, there is a strong correlation between annular radial fissures and pain formation during discography.8 Studies reveal that 70% of fissures reaching to one-third of the exterior segment of the annulus were closely related to pain generation.6 Radial fissures cause the migration of nucleus pulposus matrix to the exterior annulus and this induces nerve in-growth into the delaminated regions. It has been observed that at least some of this neo-innervation plays a role in pain generation.9 However; it is difficult to establish a correlation between the radiological findings of disc disease and the severity of low back pain. This is because minimal symptoms are present in many patients with radiological symptoms of disc disease; too severe pain may be present in some patients bearing no radiological evidences.10
Patients with over 3 months of ongoing chronic discogenic pain unfortunately do not respond well to conservative treatment methods alone. These patients can sometimes become addicted to medication while trying to manage the pain that restricts their quality of life to a large extent. At other times, they may be obliged to choose radical solutions like surgical spinal fusion and artificial disc replacement that have unproven efficacy.9 One of the treatment methods developed for the treatment of such patients, and considered as an intermediate step, is disc-heating procedures. One of these methods, IDET was introduced by Saal and Saal in 2000.19 IDET is a method that uses controlled thermal energy distributed by a catheter placed intradiscally. It has been supposed that IDET shows its effects by causing the coagulation of nociceptors and denaturation of the collagen at posterior and/or posterolateral annulus. However, temperature of the tissue should reach a minimum of 45oC to see this effect. There are doubts as to whether or not IDET creates this degree of heat.20,21
One other problem about IDET is its questionable effectiveness. Perhaps the most interesting study on this subject is the one conducted by Freeman et al.7 This randomized, double-blind, controlled study was published in 2005, and demonstrated that IDET had no superior results over a placebo. Although the extraordinarily distinct result in this study may be tied to inappropriate patient selection9 and the technique applied10; it is arguable that IDET was effective in appropriately chosen small patient groups.12
IDET is a method that is technically difficult to apply. This difficulty in application requires sufficient experience and skill. Although the available literature on IDET emphasizes that it is a safe method, serious complications such as catheter breakage, vertebral osteonecrosis and cauda equina syndrome were also reported.7
TDB is a new method in the treatment of chronic discogenic pain. Despite the presence of insufficient number of studies about its efficacy and safety, the preliminary findings show that this method was effective12,15 and safe17 in a selected group of patients. Kapural et al.12, in a clinical study they published, prospectively investigate the effectiveness of TDB in fifteen patients. They used VAS and opioid consumption to evaluate pain, and the ODI and Short Form (SF)-36 questionnaire to evaluate physical functions. They reported a statistically significant improvement in the VAS, ODI, SF-36 PF and SF-36 BP scores of patients 6 months after the treatment. Despite an average of 20 mg decrease in opioid consumption at the end of 6 months, the authors report that this decrease does not constitute a statistically significant difference. While the patients report a ≥50% decrease in the pain scores of seven out of 13 patients who completed the study, they underlined that none of their patients developed any complications related to the intervention. We, in this study, found that there were statistically significant improvements compared to initial values in our patients' VAS and ODI scores. While the rate of our patients reporting a ≥50% decrease in their pain at 6 month after treatment was 57.1%, the rates of patients reporting a decrease of at least two points in VAS values and 10 points in ODI scores were same, and are 78.6%. While 71.4% of our patients were satisfied about the intervention, we observed no complications related to the intervention in any of our patients.
The most important shortcoming and weakness of this study is that it demonstrates preliminary results covering only fifteen patients. Therefore, the outcomes of this study may not be generalized to the general public. However, we are of the opinion that our study is important in that it gives preliminary information on TDB's short-term effectiveness and safety.
CONCLUSION
This study showed that compared with Intradiscal Electrothermal Therapy (IDET), TransDiscal Biacuplasty is a much more easily applicable method. In addition, TransDiscal Biacuplasty may be as effective as IDET, and is possibly safer than IDET.
CONFLICT OF INTEREST
The authors have declared that no conflict of interest exists.
References
1. Carey TS, Garrett JM, Jackman AM. Beyond the good prognosis. Examination of an inception cohort of patients with chronic low back pain. Spine. 2000;25:115-20
2. Nachemson AL. Newest knowledge of low back pain. A critical look. Clin Orthop. 1992;279:8-20
3. Schwarzer AC, Aprill CN, Derby R. et al. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995;20:1878-83
4. Smith SE, Darden BV, Rhyne AL. et al. Outcome of unoperated discogram-positive low back pain. Spine. 1995;20:1997-2000
5. Deyo RA, Nachemson A, Mirza SK. Spinal fusion surgery—the case for restraint. N Engl J Med. 2004;350:722-6
6. Singh V. Intradiscal Electrothermal Therapy: A Preliminary Report. Pain Physician. 2000;3:367-73
7. Freeman BJ, Fraser RD, Cain CM. et al. A randomized, double-blind, controlled trial: intradiscal electrothermal therapy versus placebo for the treatment of chronic discogenic low back pain. Spine. 2005;30:2369-77
8. Karasek M, Bogduk N. Twelve month follow-up of a controlled trial of intradiscal thermal anuloplasty for back pain due to internal disc disruption. Spine. 2000;25:2601-7
9. Maurer P, Block JE, Squillante D. Intradiscal electrothermal therapy (IDET) provides effective symptom relief in patients with discogenic low back pain. J Spinal Disord Tech. 2008;21:55-62
10. Nunley PD, Jawahar A, Brandao SM. et al. Intradiscal electrothermal therapy (IDET) for low back pain in worker's compensation patients: can it provide a potential answer? Long-term results. J Spinal Disord Tech. 2008;21:11-8
11. Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain. A prospective outcome study with minimum 1-year follow-up. Spine. 2000;25:2622-7
12. Kapural L, Ng A, Dalton J. et al. Intervertebral disc biacuplasty for the treatment of lumbar discogenic pain: results of a six-month follow-up. Pain Med. 2008;9:60-7
13. Pauza KJ, Howell S, Dreyfuss P. et al. A randomized, placebo controlled trial of intradiscal electrothermal therapy for the treatment of discogenic low back pain. Spine J. 2004;4:27-35
14. Freeman BJ, Fraser RD, Cain CM. et al. A randomized, double blinded, controlled trial: intradiscal electrothermal therapy versus placebo for the treatment of chronic discogenic low back pain. Spine. 2005;30:2369-77
15. Kapural L, Mekhail N. Novel Intradiscal Biacuplasty (IDB) for the Treatment of Lumbar Discogenic Pain. Pain Practice. 2007;7:130-4
16. Pilcher TA, Sabford AL, Saul JP. et al. Convective cooling effect on cooled-tip catheter compared to large-tip catheter radiofrequency ablation. Pacing Clin Electrophysiol. 2006;29:1368-74
17. Kapural L, Mekhail N, Hicks D. et al. Histological changes and temperature distribution studies of a novel bipolar radiofrequency heating system in degenerated and nondegenerated human cadaver lumbar discs. Pain Med. 2008;9:68-75
18. Andersson GB, Mekhail NA, Block JE. Treatment of intractable discogenic low back pain. A systematic review of spinal fusion and intradiscal electrothermal therapy (IDET). Pain Physician. 2006;9:237-48
19. Saal JS, Saal JA. Management of chronic discogenic low back pain with a thermal intradiscal catheter: a preliminary report. Spine. 2000;25:382-8
20. Shah RV, Lutz GE, Lee J. et al. Intradiskal electrothermal therapy: a preliminary histological study. Arch Phys Med Rehabil. 2001;82:1230-7
21. Freeman BJ, Walters RM, Moore RJ. et al. Does Intradiscal Electrothermal Therapy denervate and repair experimentally induced posterolateral annular tears in an animal model? Spine. 2003;28:2602-8
Author contact
![]() Corresponding author: HAKTAN KARAMAN, Dicle Universitesi Tıp Fakultesi Anestezi A.D. 21280 Diyarbakir-TURKEY. Phone: +90 412 248 80 01/4369; Fax: +90 412 248 85 23; E-mail: haktanedu.tr
Corresponding author: HAKTAN KARAMAN, Dicle Universitesi Tıp Fakultesi Anestezi A.D. 21280 Diyarbakir-TURKEY. Phone: +90 412 248 80 01/4369; Fax: +90 412 248 85 23; E-mail: haktanedu.tr

 Global reach, higher impact
Global reach, higher impact