Impact Factor
ISSN: 1449-1907
Int J Med Sci 2010; 7(6):391-394. doi:10.7150/ijms.7.391 This issue Cite
Research Paper
Prevalence of Overactive Bladder, its Under-Diagnosis, and Risk Factors in a Male Urologic Veterans Population
1. SUNY Downstate Medical School, Department of Urology, Brooklyn, NY, USA
2. Wayne State University School of Medicine, Department of Pathology , Detroit, MI, USA
Received 2010-4-4; Accepted 2010-9-9; Published 2010-11-12
Abstract
Purpose: We assess the prevalence of overactive bladder (OAB) and its risk factors in a male urologic veterans population. Materials and Methods: Validated self-administered questionnaire was prospectively given. Results: Among 1086 patients, OAB was present in 75%, of which 48% had not been diagnosed/treated. The risk of OAB increased with age. OAB was not associated with BMI, smoking, race, diabetes, CHF, and COPD. Conclusions: The prevalence of OAB in this population is under-diagnosed and under-treated.
Keywords: overactive bladder, OAB, incontinence, male, urology, veterans
INTRODUCTION
Recent international population and non-population studies reported overactive bladder (OAB) in 10-17% of the adult population, depending on sex.1,2,3,4 In the U.S., a population-based study reported that 16.0% of men and 16.9% of women experienced OAB.5 No study has examined the prevalence of OAB in the urologic population, which is expected to be much higher. Some studies have reported association of OAB with age (men and women), body mass index - BMI (female), menopause (female), constipation (female), episiotomy (female), and beer consumption (men). 2, 6,7,8
In this prospective cohort study, we assess the prevalence of OAB in urologic male veterans population, the need for OAB screening, and risk factors for OAB.
METHODS
An IRB-approved self-administered questionnaire on urinary symptoms was given to male patients who visited the general urology outpatient clinic at a Veterans Administration hospital in Brooklyn, NY. It included questions on lower urinary tract symptoms (LUTS) with 0-5 point scale and on quality of life with 0-6 (best to worst) point scale (based on a modified validated Overactive Bladder 8-question Screener (OAB-V8)9). Questions on LUTS included urinary frequency (2 questions), urgency (2), nocturia (1), incontinence (2) and emptying (1). The questionnaire also included medical and surgical history, demographic data, BMI, medications and visit diagnosis.
OAB-V8 total score that was equal to or greater than 6 for men was defined as OAB positive. Subsequent questionnaires from the same patient were excluded.
To determine the relationship between OAB and other factors (age, BMI, smoking, race, diabetes, hypertension, congestive heart failure, chronic obstructive pulmonary disease, diuretic medications and hepatitis), covariates were first individually evaluated using the chi-square test. Statistically significant (p < .05) covariates were retained for odds ratio analysis. Patients were excluded from a specific analysis if they did not report on the variable to be analyzed. Results are presented as odds ratio and 95% confidence interval (95% CI) 10. Statistical analyses were performed using Stata 8.2 (StataCorp, College Station, TX).
RESULTS
Among the male patients, 1086 completed the questionnaire. Table 1 summarizes the demographic data. Mean age was 68 years old (quartile range: 59-77). The major ethnicities were European American (44%), African American (37%) and Hispanic American (11%).
Demographics
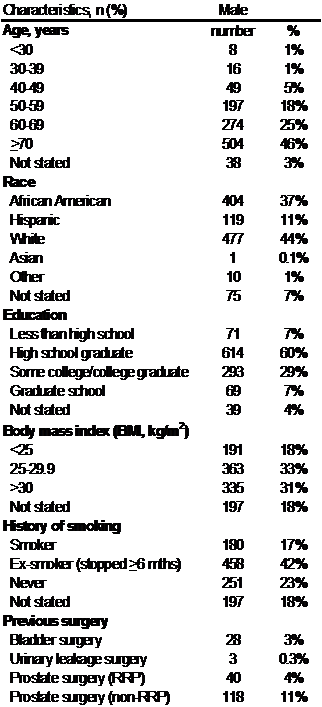
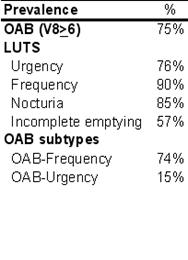
OAB was present in 75%. Among those surveyed with OAB, 48% had not been diagnosed with or treated for OAB, LUTS or benign prostatic hypertrophy (BPH). Those with OAB had a worse quality of life score. Mean quality of life score for those with OAB was 3.4 of 6, and those without OAB 1.6. Furthermore, 59% reported urge incontinence, 76% urgency, 90% frequency and 85% nocturia.
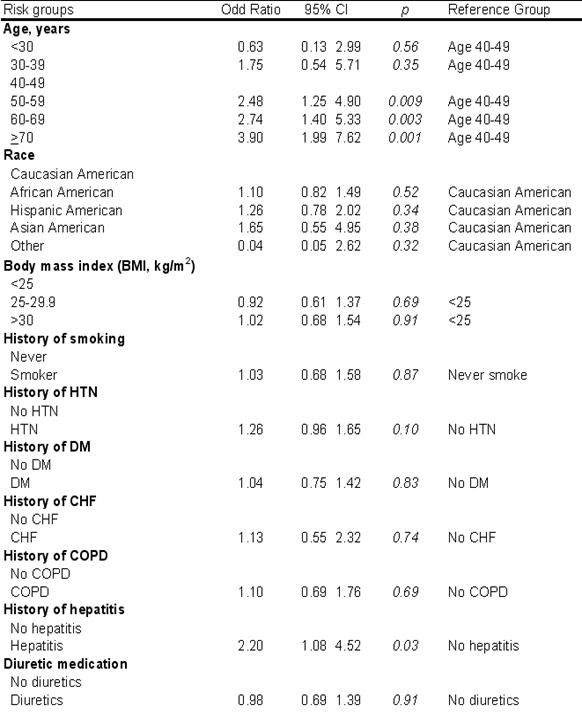
There was no association of OAB with BMI (p=0.61), smoking (p=0.87), race (p=0.32), diabetes (p=0.83), hypertension (p=0.10), congestive heart failure (p=0.74), chronic obstructive pulmonary disease (p=0.69), and diuretic medications (p=0.91). The risk of OAB increased with age: 49% in men aged 40-49 years to 79% in men aged 70-79 years (p<0.001, OR=3.9). Interestingly, there was a statistically significant association between OAB and hepatitis (p=0.03, OR=2.2). See Table 3.
Prevalence of OAB, LUTS and OAB subtypes.
DISCUSSION
The prevalence of OAB in men has been reported to be 10.2-16.0%. It is expected to be much higher in the urologic setting since urinary complaint is a common reason for urologic visit. Our study found that 75% of those surveyed, experienced OAB. This is almost five fold higher than that reported for the general population. Since OAB is a compilation of lower urinary tract symptoms, the prevalence of LUTS should be higher. Irwin et al.2 in their 5-country population study reported the prevalence of any LUTS to be 62.5% whereas the prevalence of OAB to be 10.8%. Our study found that 95% reported urinary frequency and 85% nocturia. The increase in our study is consistent with Irwin et al.'s epidemiologic study.
Although a higher prevalence of OAB is expected in our study population, the increase may also be compounded by variation in OAB definition. Most reported population studies had used the 2002 International Continence Society definition of OAB. Our study is based on a validated OAB screener questionnaire (OAB-V8). As with any screening tool, the sensitivity should be high but specificity may not be high. The OAB-V8 questionnaire has only been validated in a primary care setting. Validation in a high risk population is still pending.
Our study showed that among those with OAB, only 52% had been diagnosed with or treated for urinary symptoms (OAB, LUTS and/or BPH). Furthermore, those with OAB had a worse quality of life score. Mean quality of life score for those with OAB was 3.4 of 6, and those without OAB 1.6. Thus, the 48% of men with OAB that are undiagnosed or untreated may benefit from better detection and treatment initiation. The OAB-V8 questionnaire is a possible effective and fast screening tool.
Our study also examined the risk factors for OAB in men. We found that OAB increased with age: 49% in men aged 40-49 years to 79% in men aged 70-79 years (p<0.001, OR=3.9). This is consistent with previous epidemiologic studies. Our study also found an association between OAB and hepatitis (OR=2.2, p=0.03). It is uncertain how hepatitis relates to OAB. As such additional epidemiologic studies are needed in this regard. Unlike previous studies by Teleman et al.8, we found no association between OAB and BMI. However, patients in that study were all female. We also found no association with smoking, race, diabetes, hypertension, congestive heart failure, chronic obstructive pulmonary disease, and diuretic medications.
Risk factors for OAB.
CONCLUSION
The prevalence of OAB in the male urologic veterans is almost five fold higher than that reported for the general population. OAB is under-diagnosed and under-treated. This patient population may benefit from routine screening. Furthermore, our study shows that OAB is associated with age and a history of hepatitis.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Temml C, Heidler S, Ponholzer A, Madersbacher S. Prevalence of the overactive bladder syndrom by applying the International Continence Society Definition. Eur Urol. 2005;48:622
2. Irwin D, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S. et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306
3. Herschorn S, Gajewski J, Schulz J, Corcos J. A population-based study of urinary symptoms and incontinence: the Canadian Urinary Bladder Survey. BJU Int. 2008;101:52
4. Milsom I, Abrams P, Cardozo L, Roberts RG, Throff J, Wein A. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87:760
5. Stewart W, Rooyen JV, Cundiff G, Abrams P, Herzog S, Corey R. et al. Prevalence and burden of overactive bladder in the United States. J Urol. 2003;20:327
6. Dallosso HM, Matthews RJ, McGrother CW, Donaldson MM, Shaw C, Leicestershire MRC. The association of diet and other lifestyle factors with the onset of overactive bladder: a longitudinal study in men. Public Health Nutr. 2004;7:885
7. Zhang W, Song Y, He X, Huang H, Xu B, Song J. Prevalence and risk factors of overactive bladder syndrome in Fuzhou Chinese women. Neurourol Urodyn. 2006;25:717
8. Teleman PM, Lidfeldt J, Nerbrand C, Samsioe G, Mattiasson A, WHILA study group. Overactive bladder: prevalence, risk factors and relation to stress incontinence in middle-aged women. BJOG. 2004;111:600
9. Coyne K, Margolis M, Zyczynski T, Elinoff V, Roberts RG. Validation of an OAB screener in a primary care patient population in the US; Poster. Paris, France: International Continence Society Annual Meeting. 2004
10. Cheung WW, Khan NH, Choi KK, Bluth MH, Vincent M. Prevalence, evaluation and management of overactive bladder in primary care. BMC Family Practice. 2009;10:8
Author contact
![]() Corresponding author: Wellman W Cheung, MD, SUNY Downstate Medical Center, Departments of Urology and Obstetrics/Gynecology, 450 Clarkson Avenue, Brooklyn, NY 11230. Email: wellman.cheungedu
Corresponding author: Wellman W Cheung, MD, SUNY Downstate Medical Center, Departments of Urology and Obstetrics/Gynecology, 450 Clarkson Avenue, Brooklyn, NY 11230. Email: wellman.cheungedu

 Global reach, higher impact
Global reach, higher impact