3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2010; 7(5):248-250. doi:10.7150/ijms.7.248 This issue Cite
Case Report
Post-traumatic glioma: Report of one case and review of the literature
Department of Neurosurgery, Second Affiliated Hospital, College of Medicine, Zhejiang University, # 88 Jiefang Road, Hangzhou City, 310009, PR China
Received 2010-6-26; Accepted 2010-7-23; Published 2010-7-29
Abstract
We report one case of brain glioma that developed in the scar of an old brain trauma. A 45-year-old man who presented with seizures; MRI showed a large mass in the right temporal region. Surgical biopsy showed a glioblastoma multiforme. The patient had suffered a cranial trauma in a road accident 10 years previously with an intracerebral hematoma in the right temporal region. This case fulfills the established criteria for a traumatic origin of brain tumors and adds further support to the relationship between cranial trauma and the onset of glioma. As stated by other authors, an association between head trauma and brain tumor risk cannot be ruled out and should be studied further.
Keywords: head trauma, post-traumatic glioma
1. Introduction
Until now, there are only a few cases in which the relationship between a previous traumatic event and the occurrence of a brain glioma is unequivocally demonstrated on the basis of well accepted criteria. Recently, Elisa Anselmi et al. 1 reported two patients who developed brain gliomas in the scar of an old brain injury meet all the criteria for a causal relationship between head trauma and glioma; these cases did support the theory of a causal relationship between trauma and gliomas. Here we report one case of glioma that developed in a patient with a previous head trauma, which adds further support to the causal relationship between brain trauma and gliomas.
2. Case report
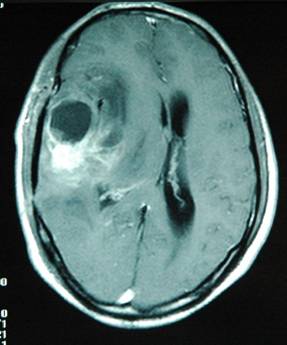
A previously healthy 45-year-old man presented with seizures and expressive aphasia. He was admitted to our hospital. Magnetic resonance imaging (MRI) documented a large contrast-enhancing lesion in the right temporal region (Fig. 1). The mass histological examination revealed a glioblastoma multiforme. About 10 years earlier the patient had suffered a cranial trauma in a road accident when he traveled in another city. After the trauma he had been unconscious for 3 days and CT scan demonstrated an intracranial hematoma in the right temporal lobe at the site of the subsequent glioblastoma. The intracranial hematoma was treated conservatively at that time. After the diagnosis of the glioblastoma multiforme the patient was treated with radiotherapy and chemotherapy, but he died seven months later.
3. Discussion
Although epidemiological studies do not support a definitive connection between head injury and intracranial glioma2, there have been a few case reports of post-traumatic gliomas. As has been reported recently1, it must be emphasized that some of the described cases with post-traumatic glioma did not fulfill the criteria suggested by zulch3 for a relationship between trauma and tumor, only a few authors have provided definite evidence of the causative role of trauma 4.
Zulch 3 in 1965 suggested the following criteria for the acceptance of a causal relationship between trauma and the onset of cerebral tumors:
- The patient must have been in good health before suffering the head injury.
- The below must be severe enough to cause brain contusion and a secondary reparative process.
- The location of the impact and the tumor should correspond exactly one to the other.
- There should be a time interval between trauma and the appearance of the tumor of at least 1 year, a longer latent period increasing the likelihood of a causal relationship.
- The presence of the tumor must be proved histologically.
- Trauma should consist of an external force.
Manuelidis 5 in 1972 added three more criteria:
- The traumatized brain must also be proved histologically.
- Bleeding, scars and edema secondary to the presence of the tumor must be clearly differentiated from that caused by trauma.
- Tumor tissue should be in direct continuity with the traumatic scar, not merely in its vicinity or separated by a narrow zone of healthy or slightly altered brain tissue.
The stringent criteria for diagnosing a posttraumatic glioma proposed by Zulch et al. 3 and Manuelidis et al. 5 require histopathological confirmation. These criteria were established in the pre-CT (computed tomography) era. The recent cases of posttraumatic glioma that have been reported show CT scans at the time of the trauma demonstrating significant injury and the follow-up scans demonstrating tumor at the same site4. With the routine use of CT and magnetic resonance imaging (MRI), some of the pathologic criteria can be replaced or supplemented by imaging criteria. CT/MRI, which elegantly reveal the severity and location of the traumatic brain injury and the subsequent formation of a neoplasm at the same site, can provide convincing evidence for the traumatic causation of a brain tumor.
Our case fulfill all the criteria defined by Zulch and two of the three criteria of Manuelidis because the intracerebral hematoma secondary to trauma was not histologically verified; it must be emphasized, however, that CT scan documented the absence of tumor at the time of the brain injury.
We suggest that these conditions for the acceptance of a causal relationship between cranial trauma and brain tumor study are the following: (1) the patient had been in good health before suffering the head injury, and early brain CT was negative; (2) the blow was severe and caused brain contusion or intracranial hematoma with a secondary reparative process; (3) the location of the impact and the occurrence of the tumor corresponded exactly one to the other; and (4) there was a more than one year interval between trauma and the appearance of the tumor.
As regards the pathogenesis of post-traumatic glioma, the regenerative and scarring processes secondary to the trauma may in some rare instances stimulate neoplastic proliferation; for these reasons it is important that the tumor arises at the site of the old scar to demonstrate a relationship between trauma and tumor6. If the tumor arises at different site of the old lesion, should be coincidence7. The fact that epidemiological studies have not shown marked increase of the relative risk may reflect the fact that the association, if it exists, is not a direct one. The mechanism of post-traumatic brain cancer is unclear. Experimental data have shown that trauma can act as a cocarcinogen in the presence of an initiating carcinogen 2. It was hypothesized that cells damaged by the initiating carcinogen proliferated as a natural result of the trauma, leading to tumor formation. Trauma probably acts as a cocarcinogen in the presence of an initiating carcinogen, i.e. it may induce the proliferation of “initiated ” cells.
MRI scan of the head show a large temporal mass secondary to the glioblastoma at the site of the previous intracerebral hematoma.
4. Conclusion
An association between head trauma and brain tumor risk cannot be ruled out and should therefore be studied further. Post-CT/MRI era should have more convenient conditions to study. Large study populations are imperative because of the relatively low prevalence of head injuries and the low incidence of brain tumors.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Anselmi E, Vallisa D, Berte R. et al. Post-traumatic glioma: Report of two cases. Tumori. 2006;92:175-7
2. Preston-Martin S, Pogoda JM, Schlehofer B. et al. An international case-control study of adult glioma and meningioma: the role of head trauma. Int J Epidemiol. 1998;27:579-586
3. Zulch KJ. Brain tumors: Their biology and pathology, 2nd edition. New York, USA: Springer-Verlag Publisher. 1965:51-58
4. Henry PT, Rajshekhar V. Post-traumatic malignant glioma: case report and review of the literature. Br J Neurosurgery. 2000;14:64-7
5. Manuelidis EH. Glioma in trauma. In: (ed.) Minckler J. Pathology of the Nervous System. New York, USA: McGraw Hill Publisher. 1972
6. Di Trapani G, Carnevale A, Scerrati M. et al. Post traumatic malignant glioma. Report of a case. Ital J Neurol Sci. 1996;17:283-286
7. Hu XW, Zhang YH, Wang JJ. et al. Angiocentric glioma with rich blood supply. J Clin Neurosci. 2010;17(7):917-8
Author contact
![]() Corresponding author: Tel./fax: +86 15157161309. E-mail: liuweiguo618com
Corresponding author: Tel./fax: +86 15157161309. E-mail: liuweiguo618com

 Global reach, higher impact
Global reach, higher impact