Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(5):274-279. doi:10.7150/ijms.6.274 This issue Cite
Review
Mechanical complications and reconstruction strategies at the site of hip spacer implantation
1. Klinik für Orthopädie und Orthopädische Chirurgie, Universitätskliniken des Saarlandes, Homburg/Saar, Germany
2. Chirurgisch-Orthopädisches Zentrum Illingen/Saar, Germany
Received 2009-8-1; Accepted 2009-9-2; Published 2009-9-3
Abstract
Over the past two decades antibiotic-impregnated hip spacers have become a popular procedure in the treatment of hip joint infections. Besides infection persistence and/or reinfection, major complications after hip spacer implantation include spacer fracture, -dislocation, and bone fracture. Moreover, in cases with extensive loss of femoral and/or acetabular bone alternative reconstructive techniques should be used for a stable spacer fixation and prevention of fractures or dislocations. The present article reviews the different types of spacer fractures and dislocations and offers some suggestions about reconstructive techniques for management of extensive loss of femoral and/or acetabular bone at the site of hip spacer implantation.
Keywords: hip spacers, spacer fracture, spacer dislocation, femoral fracture, reconstruction.
Introduction
Over the past two decades antibiotic-impregnated hip spacers have become a popular procedure in the treatment of hip joint infections with reported success rates of > 90 % [1]. Although initially developed for the management of infected total hip arthroplasties, hip spacers have been successfully used also in the treatment of bacterial coxitis or infections of the proximal femur after osteosynthesis [4]. The major advantages of a hip spacer implantation are: (i) immediate treatment of the infection source by locally reaching high antibiotic levels, (ii) maintance of joint mobility, (iii) limitation of scar formation, (iv) absence of soft tissue contraction (usually resulting to a leg length discrepancy) and (v) facility for reimplantation [1].
One of the major complications after hip spacer implantation regards mechanical complications. Spacer fractures and dislocations as well as femoral fractures may endanger the functional outcome and impede the later prosthesis reimplantation. Although several reports have described these complications, the exact incidence of these mechanical complications is still unknown due to insufficient documentation or differences in the precise definition of spacer dislocations. Moreover, in cases with extensive loss of bone, either on the femoral or acetabular side, there exist no consensus as to which reconstructive procedure should be performed that guarantees an infection eradication and has a minimal risk regarding the abovementioned mechanical complications.
In the past 10 years approximately 100 patients have been treated in our department by hip spacer implantation due to various hip joint infections. In this article, we report our experience in the prophylaxis and treatment of mechanical complications at the site of a hip spacer implantation and suggest some reconstructive techniques for management of extensive loss of femoral and/or acetabular bone.
Mechanical complications and reconstruction strategies
The exact rate of mechanical complications following hip spacer implantation remains unknown. Despite numerous reports about these complications, only Leunig and colleagues tried to interpret and explain these findings [6]. The authors have recognized that the geometrical form of the spacer plays an important role. In spacers which were free of complications the neck to head-ratio was significantly lower (0.76±0.05) than in those with dislocations (0.96±0.19). A second factor associated with failure was an insufficient deep anchorage in the intramedullary canal, being 22±33 mm in the failure group, while complication-free spacers were on average attached to a depth of 57±41 mm.
Generally, a spacer dislocation might occur if
- the patient is not compliant,
- partial weight bearing of the operated extremity cannot be tolerated,
- the spacer is insufficiently fixated onto the proximal femur,
- the size of the spacer head is too small,
- large osseous defects of the acetabulum do not allow for a normal spacer articulation, and
- a muscular insufficiency is present.
Moreover, the term “spacer dislocation” may describe two different kinds of dislocation. A dislocation may occur in the femoral canal due to an insufficient fixation technique, but the spacer head may remain in such cases in the acetabulum cup. The solution for this problem is to improve the femoral fixation of the spacer stem. Alternatively to that and at stable femoral fixation, the spacer itself may dislocate out from the hip socket. In these cases, specific attention should be paid on whether a wrong motion of the hip joint led to the dislocation, the spacer head is too small or extensive acetabular defects do no provide enough primary stability for a normal spacer articulation. In the former cases, the hip joint can be reduced and a conservative treatment in an orthesis can be utilized.
Depending on the particular cause, treatment options may strongly vary. In case of patient incompliance or inability to put partial weight bearing on the operated extremity, the patient should be rather considered as a candidate for a resection arthroplasty and not for a spacer implantation. For prevention of any spacer dislocation due to an insufficient fixation technique onto the proximal femur, a simple “press fit” method should be avoided (Figure 1). Alternatively, a partial (Figure 2) or normal cementation of the spacer into the femoral canal provides the advantage of rotational and axial stability [3]. A normal cementation has the disadvantage in comparison with the partial cementation that all cement debris have to be removed from the femoral canal during the later prosthesis reimplantation, and that during removal of the prosthesis stem osseous defects might occur. Recently, the “glove”-technique has been described as new method for femoral fixation of hip spacers [3]. This method provides a stable fixation onto the proximal femur at facilitating the spacer's explantation since the spacer can be removed at one piece and there is no need for removal of any cement debris compared with other normal cementation techniques.
In cases with muscular insufficiency or large acetabular defects, the spacer should not be implanted as a hemiarthroplasty, but rather as a total arthroplasty, consisting of a spacer stem and a cup (Figure 3). This is also of benefit in cases where the spacer head is too small for the acetabulum cavity. Since not every department has molds for production of spacers in different sizes or lengths or the costs for commercially available hip spacers are extremely high, the orthopaedic surgeon is commonly faced with the dilemma: should a larger, hand-molded spacer head be implanted (which, however, has the disadvantage of an inferior articulation due to the uneven head surface and form) or, alternatively, a spacer cup is inserted into the acetabulum. We recommend the second option. This implantation technique also offers the advantage of a prevention of a spacer migration into the pelvis (Figure 4) beside a normal articulation and prevention of any spacer dislocation. Hereby, the cement-cement articulation promotes the emergence of high local antibiotic concentrations due to the continuous friction of the articulating components. Cement debris can be then easily removed at the time of the prosthesis reimplantation via pulsatile lavage and debridement. However, in some cases with a combined muscular insufficiency and large acetabular defects a spacer dislocation might still occur. These cases should be also considered as candidates for a resection arthroplasty.
A spacer fracture can be either symptomatic or asymptomatic depending on the fracture localisation. Symptomatic fractures (Figure 5) are usually the consequence of a spacer neck fracture and frequently associated with a subsequent spacer head dislocation. In these cases treatment should consist of revision surgery and spacer exchange. On the other hand, asymptomatic fractures are found in the middle or lower part of the spacer stem (Figure 6) and usually require no further operative treatment.
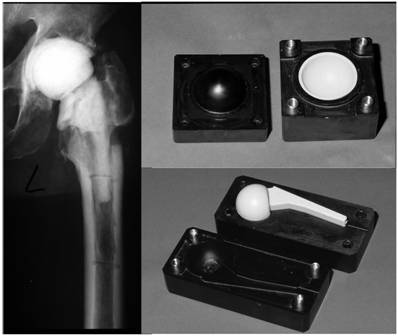
For prevention of a spacer fracture, the surgeon may consider inserting a metallic endoskeleton (Figure 7) into the spacer; however, literature data are scarce about this topic. Schöllner et al. investigated in vitro the mechanical properties of gentamicin-loaded hip spacers after insertion of Kirschner wires [7]. Stress experiments showed an average failure load of 1.6 kN. The insertion of the K-wires prevented any dislocation of the spacer fragments, but did not significantly improve the mechanical properties. Kummer et al. compared in vitro the mechanical properties of commercially available hip spacers containing a substantial stainless steel central core with experimental spacers containing Steinmann pins, intramedullary nails with two lag screws and Charnley prostheses, respectively [5]. The authors reported that all constructs based upon the Charnley prostheses and the commercial spacers did not fail at 3000 N; the other two constructs failed at significant lower loads (pins at 832 N and nails at 1275 N, respectively). To our knowledge, there are no clinical data available that have demonstrated that the insertion of a metallic endoskeleton significantly improves the mechanical properties of hip spacers or reduces the rate of mechanical complications.
Moreover, it is still unclear whether the insertion of a metallic endoskeleton has a negative influence on the pharmacokinetic properties of the spacer. Experimental data have shown that the release of commercially-impregnated antibiotics from hip spacers is significantly increased in the presence of an endoskeleton, whereas the elution of additional, incorporated antibiotics is decreased [2]. Until this question is answered, metallic endoskeletons should not be routinely inserted into hip spacers in clinical practise, but only in exceptional cases for patients with a higher fracture risk (high Body-Mass-Index, poor bone quality or osteoporosis).
Femoral fractures at the site of hip spacer implantation should be treated when an unstable joint situation results, the outcome of the surgery is endangered or the mobilisation of the patient is hereby limited. Generally, the surgical treatment of these fractures should be planned taking into consideration any further surgical revisions or the later prosthesis reimplantation. If possible, the insertion of any metallic implants should be avoided if the infection is not completely eradicated for avoidance of an infection persistence or reinfection. In difficult cases with a nonsupportive proximal femur part, the treatment's choice should be made under consideration of both infection sanitation and fracture management. In cases, where the spacer stem does not exceed 10 cm (in the majority of the cases), alternative reconstructive methods should be performed. In our experience, the use of modular prosthesis systems or long nails with an antibiotic-loaded cement mantle and a spacer head is an elegant method that treats both the fracture and the infection (Figure 8). At the time of prosthesis reimplantation, the spacer head can be easily removed and the modular prosthesis parts (neck and head) placed. This procedure offers a stable fracture treatment and facilitates the prosthesis reimplantation regarding shorter surgery time, less blood loss and no need for femoral exposure. Furthermore, this technique can be also applied in cases with large and extensive osseous defects of the proximal femur due to the prosthesis loosening where a stable fixation of the spacer to the proximal femur according to the usual fixation techniques is not possible (Figure 9). Although some hip spacers have the advantage of a long stem (e.g. PROSTALAC) [8] and can be treated to a similar manner as shown in Figure 8, not every clinic has these spacers in hold; the above mentioned technique is a noble alternative to these constructs.
In conclusion, there exist several parameters and factors that affect the mechanical properties of a hip spacer in vivo. Knowledge about these parameters may assist the physician to prevent and sufficiently treat such complications. Future studies should investigate the ideal geometrical form for a hip spacer, enhance the fixation techniques onto the proximal femur and evaluate the effect of a metallic endoskeleton on the pharmacokinetic properties of the interim prosthesis.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Anagnostakos K, Fürst O, Kelm J. Antibiotic-impregnated PMMA hip spacers: current status. Acta Orthop. 2006;77:628-37
2. Anagnostakos K, Kelm J, Grün S, Schmitt E, Jung W, Swoboda S. Antimicrobial properties and elution kinetics of linezolid-loaded hip spacers in vitro. J Biomed Mater Res B Appl Biomater. 2008;87:173-8
3. Anagnostakos K, Köhler D, Schmitt E, Kelm J. The „glove“-technique: a modified method for femoral fixation of antibiotic-loaded hip spacers. Acta Orthop. in press
4. Hsieh PH, Chang YH, Chen SH, Shih CH. Staged arthroplasty as salvage procedure for deep hip infection following intertrochanteric fracture. Int Orthop. 2006;30:228-32
5. Kummer FJ, Strauss E, Wright K, Kubiak EN, Di Cesare PE. Mechanical evaluation of unipolar hip spacer constructs. Am J Orthop. 2008;37:517-8
6. Leunig M, Chosa E, Speck M, Ganz R. A cement spacer for two-stage revision of infected implants of the hip joint. Int Orthop. 1998:209-14
7. Schöllner C, Fürderer S, Rompe JD, Eckhardt A. Individual bone cement spacers (IBCS) for septic hip revision - preliminary report. Arch Orthop Trauma Surg. 2003;123:254-9
8. Wentworth SJ, Masri BA, Duncan CP, Southworth SB. Hip prosthesis of antibiotic-loaded acrylic cement for the treatment of infections following total hip arthrioplasty. J Bone Joint Surg Am. 2002;84:123-8
Figures
Articulating hip spacer in situ, the spacer stem is inserted into the femur according to a “press-fit” method.

Articulating hip spacer in situ, the partial cementation of the spacer onto the proximal femur provides a rotational stability; at prosthesis reimplantation, the spacer can be removed at one piece, leaving no cement particles in the femoral canal.

Articulating hip spacer consisting of a spacer cup and -stem.
Spacer migration into the pelvis due to acetabular defects.

Symptomatic spacer neck fracture with dislocation in situ.

Asymptomatic spacer fracture localised in the middle part of the spacer stem with no dislocation of the spacer.

Antibiotic-loaded hip spacer with a metallic endoskeleton for enhancement of the mechanical properties.

Left: Femoral fracture at the site of hip spacer implantation. Right: Treatment consisted of spacer removal, and insertion of a cement-coated modular prosthesis with a spacer head. The cement mantle of the prosthesis is also antibiotic-loaded according to the sensitivity profile of the causative organism. After infection eradication, the spacer head has been removed and a metallic head with an acetabular cup implanted. This procedure offers a stable fracture treatment and facilitates the prosthesis reimplantation regarding shorter surgery time, less blood loss and no need for femoral exposure. The remaining intrapelvic cement has no disadvantage regarding the infection eradication and might be associated with severe intraoperative complications in case of a removal trial.
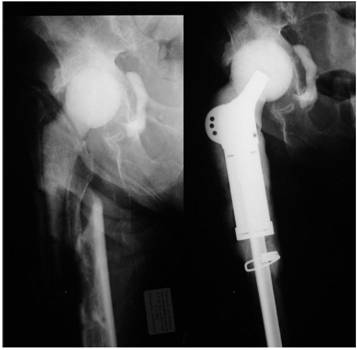
Large osseous defect of the proximal femur following extensive prosthesis loosening. Treatment consisted of prosthesis removal, debridement, pulsatile lavage, and insertion of a long femoral nail with an antibiotic-loaded cement mantle and a spacer on top.

Author contact
![]() Correspondence to: Dr. Konstantinos Anagnostakos, Klinik für Orthopädie und Orthopädische Chirurgie, Universitätskliniken des Saarlandes, Kirrbergerstr. 1, D-66421, Homburg/Saar, Germany. Tel.: 0049-6841-1624520; Fax: 0049-6841-1624516; e-mail: k.anagnostakosde
Correspondence to: Dr. Konstantinos Anagnostakos, Klinik für Orthopädie und Orthopädische Chirurgie, Universitätskliniken des Saarlandes, Kirrbergerstr. 1, D-66421, Homburg/Saar, Germany. Tel.: 0049-6841-1624520; Fax: 0049-6841-1624516; e-mail: k.anagnostakosde

 Global reach, higher impact
Global reach, higher impact