3.2
Impact Factor
ISSN: 1449-1907
Int J Med Sci 2009; 6(4):160-167. doi:10.7150/ijms.6.160 This issue Cite
Research Paper
Determinants of improvement in quality of life of alcohol-dependent patients during an inpatient withdrawal programme
Centre de Traitement des Addictions, Hôpital Emile Roux, Assistance Publique-Hôpitaux de Paris, 94450 Limeil-Brévannes, France
Received 2009-3-4; Accepted 2009-5-15; Published 2009-5-18
Abstract
Background: To investigate the improvement in quality of life (QoL) of alcohol-dependent patients during a 3-week inpatient withdrawal programme, and to identify the sociodemographic, clinical and alcohol-related variables associated with baseline QoL on admission and with improvement of QoL during residential treatment.
Methods: This prospective, observational study included 414 alcohol-dependent patients, hospitalised for a period of 3 weeks. QoL was measured on admission and at discharge using the French version of the Medical Outcome Study SF-36. The mean scores for each dimension and for the Physical and Mental Component Summary scores were calculated.
Results: The mean scores per dimension and the mean Physical and Mental Component Summary scores were significantly lower on admission than at discharge; the lowest scores being observed for social functioning and role limitations due to emotional problems. At discharge, the mean scores per dimension were similar to those observed in the French general population. Female gender, age >45 years, living alone, working as a labourer or employee, somatic comorbidity, and the existence of at least five criteria for alcohol dependence according to the DSM-IV classification were associated with a low Physical Component Summary score on admission; psychiatric comorbidity, the presence of at least five DSM-IV dependence criteria, smoking and suicidality were associated with a low Mental Component Summary score on admission. The increase in Physical and Mental Component Summary scores during hospitalisation was more marked when the initial scores were low. Apart from the initial score, the greatest improvement in Physical Component Summary score was seen in patients with a high alcohol intake and in those without a somatic comorbidity; the increase in Mental Component Summary score was greatest in patients without psychotic symptoms and in those who abused or were dependent on illegal drugs.
Conclusion: QoL improvement after a residential treatment was related to low QoL scores at admission. Improvement in physical component of QoL was related to baseline alcohol intake and good somatic status. Improvement in mental component of QoL was related to other drugs abuse/dependence.
Keywords: alcohol-dependent patients, residential treatment, quality of life
Introduction
Alcohol dependence is a chronic disorder. If a complete cure of the disorder is generally not possible, long-term supervision of alcohol dependence is required in order to ensure that alcohol-dependent patients have the best possible state of general health. The World Health Organisation (1) has defined health not only as the absence of disease but also as a state of physical, mental and social well-being. The idea of quality of life (QoL) incorporates these dimensions and can be defined as “an individual's perception of their position in life, and in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns (1).
The alcohol use disorder, which is usually chronic, requires patients to muster all their capacities for reconstruction and adaptation. QoL, which is a concept situated between social and clinical sciences, is a pertinent indicator to evaluate the subjective experience of the patient and to quantify the psychosocial burden of alcoholism (2, 3). Measurement of a patient's QoL requires a different approach to that typically used in clinical research, where the phycian is generally responsible for rating the health condition of the patients. In quality of life research the aim is to measure the patients' subjective perception of their state of health and life using a standardised questionnaire. Subjective perceptions of the patient may indeed by quite different from the clinician's perception of the health status of the patient (4, 5). Patient-reported outcome measures such as QoL may be useful in orientating choice between different therapeutic options since effective treatment should not only improve the clinical state and prognosis of the patient but also their QoL. The initial QoL of patients can also affect the prognosis of various disease states (3).
In alcohol-dependent patients, most published reports have investigated the effects of alcohol intervention strategies on objective clinical or psychological criteria such as alcohol intake, biological variables, severity of dependence, motivation for change, somatic or psychiatric comorbidities (6, 7). However, this approach is sometimes too limited because it does not capture adequately information on how a patient adapts to treatment and lifestyle changes (8). In current practice standards, the QoL of alcohol-dependent patients is not measured systematically, even though this is relevant to the psychosocial context of the interventions and to describing how actively patients will participate in their own care (9-11). Studies dedicated to the analysis of QoL of alcohol-dependent patients have already yielded valuable information, whether measuring basal QoL, its improvement during patient care, or its influence on alcohol-dependence itself (9-20). Most of these studies have found QoL to be decreased considerably in alcohol-dependent patients, but little information is available on how QoL changes during a therapeutic intervention (9-13, 19, 21). Some studies have identified factors associated with a poor QoL at the beginning of treatment in alcohol-dependent patients but these have not been investigated in a systematic way predictors of change in QoL (13, 20). The variables associated with an improvement in QoL of patients during care and the influence of QoL on the prognosis of alcoholism are unknown (22, 23).
The aims of this study in a clinical setting was: 1) to determine the change in QoL of alcohol-dependent patients during a 3-week inpatient programme; 2) to identify the variables associated with QoL in alcohol-dependent patients before detoxification, and how they change during a 3-week inpatient programme.
Materials and methods
Population studied
The study was carried out in the Addiction Treatment Centre, Hôpital Emile Roux, Limeil-Brévannes, Paris. The study population consisted of all alcohol-dependent patients (n=414), as defined by DSM-IV criteria, who were hospitalised for a period of 3 weeks over a 30-month inclusion period. Patients who could not understand or read the questionnaires for intellectual or social-educational reasons were not included. Briefly, the inpatient therapeutic program consisted in a benzodiazepine treatment adapted to each patient alcohol withdrawal syndrome, a medical treatment of any psychiatric and somatic comorbidities, and a standardized psychosocial treatment.
Measures
In the therapeutic programme offered by the study centre, structured diagnostic interviews and questionnaires were administered routinely for evaluation of all patients.
The variables evaluated included the following: sociodemographic variables (age, gender, ethnic origin, family structure, level of education, socioprofessional group, professional activity); alcohol-related variables (alcohol consumption and number of days of abstinence during the 6 months preceding hospitalisation, duration of alcohol dependence, length of time since the first alcohol-related period of care, family history of alcoholism in the father or mother); diagnosis of abuse or dependence on other psychoactive substances, either legal (sedatives, tobacco), or illegal (opiates, cannabis, cocaine, amphetamines, solvents, hallucinogens, phencyclidine); somatic comorbidity (alcohol-related diseases, HIV, HBV, or HCV positive serologies, weight and height, Charlson index, index of functional comorbidity, psychiatric comorbidity); alcohol-induced or alcohol-independent mood disorders (major depressive episode, dysthymia, episode of mania or hypomania), alcohol-induced or -independent anxiety disorder (panic disorder, generalized anxiety disorder, social phobia, agoraphobia, obsessive-compulsive disorder), post-traumatic stress disorder, psychotic symptoms (checklist); QoL. Suicidality was defined as any suicidal thoughts in the past month or any lifetime suicide attempt.
Level of education, socioprofessional category, professional activity and family structure were defined according to the criteria used by the Institut National de la Statistique et des Etudes Economiques (INSEE), France. Alcohol consumption was assessed using a standardised questionnaire, the existence of an alcohol problem in the patient's father or mother was investigated using the F-SMAST and M-SMAST questionnaires, respectively (24). Diagnosis of abuse or dependence on alcohol or other psychoactive substances was performed using the DSM-IV criteria, assessed with the Mini-International Neuropsychiatric Interview (MINI) (25). This is a structured interview that enables any lifetime Axis 1 diagnosis of the DSM-IV. Dependence was defined by the presence of at least three of the seven diagnostic criteria. The severity of alcohol dependence was considered to be proportional to the number of DSM-IV criteria for dependence.
All somatic comorbidities were identified during the interview, irrespective of whether they were historical conditions that had resolved with or without sequalae, or current conditions that had developed progressively over the patient's lifetime. The Charlson's index was used to identify serious somatic comorbidities and assess their severity (26). Groll's index of functional comorbidity was used to reveal any chronic and/or disabling pathology (27). The presence of a somatic disease related to excessive alcohol consumption was specified. Weight and height were measured systematically during clinical examination and body mass index (BMI) was calculated.
Diagnosis of DSM-IV psychiatric comorbidities over the patients' lifetime was carried out using the MINI. For some diagnoses, disorders independent from or induced by alcohol-dependence were identified. Disorders were considered to be alcohol-independent if they had appeared before the alcohol abuse or dependence onset or after a period of abstinence of at least 1 month. Otherwise the problem was considered to have been alcohol-induced.
The QoL of patients was measured using the MOS SF-36. This questionnaire was administered to all patients on admission and at discharge; the mean time interval between the two was 19 ± 8 days.
The MOS SF-36 is the short form of a 149-item questionnaire developed during an observational study to assess the state of health of 2546 patients with chronic cardiovascular disease or diabetes, the Medical Outcome Study (MOS), carried out between 1986 and 1990 (28). The SF-36 is a self-administered generic health-related QoL profile which includes 36 items distributed across eight dimensions: 1) physical functioning (29); 2) role limitations attributable to physical problems (RP); 3) bodily pain (BP); 4) perception of general health (GH); 5) vitality (VI); 6) social functioning (SF); 7) role limitations attributable to emotional problems (RE) and 8) mental health (MH). Dimension scores are normalised in order to obtain a value between 0 and 100 inclusive (100*(score obtained - minimum score possible)/(maximum score possible - minimum score possible)), a high score indicating a good QoL (30). Two aggregate scores can be calculated from the scores for the eight dimensions, the Physical Component Summary score and the Mental Component Summary score. These two scores are also standardised by weighting the eight individual dimension scores using coefficients derived from studies carried out in the US general population (31). The upper and lower limits of these scores are 8 and 73 for the Physical Component Summary, and 10 and 74 for the Mental Component Summary (31). The SF-36 has been translated and validated in many different languages, including French. Standardised normative reference scores have been determined from studies in the French general population, allowing comparisons to be made between populations of different origins or different sociocultural backgrounds (30, 32). The SF-36 has also been used and validated in alcohol-dependent patients (13, 19).
Statistical analysis
QoL scores on admission and at discharge were compared using the Wilcoxon test. The Physical and Mental Component Summary scores were calculated for each patient on admission. Patients were categorised into three subgroups of equal size according to the value obtained for each Summary scores. The differences between the Physical and Mental Component Summary scores at discharge and on admission were calculated in order to determine the improvement in QoL of patients during the inpatient programme. Again, patients were categorised into three subgroups of equal size according to the degree of improvement observed.
Univariate analyses were carried out by comparing patients as a function of their QoL (QoL on admission, or difference in QoL between admission and discharge). Patients with poor QoL (i.e. lowest tercentile) on admission were compared with the other patients in terms of baseline variables using univariate analysis. Baseline variables were dichotomized choosing the median value as a cut off. A similar approach was used to compare patients with a large (i.e. combination of middle and higher tercentiles) vs low improvement in QoL. Quantitative variables were compared by ANOVA and frequencies were compared using the Chi-square test. Normally distributed quantitative variables are expressed as means ± SEM. Non-normally distributed variables were expressed as median and range. Multivariate logistic regression analyses were used to test the independent contribution of variables to QoL after adjustment for confounding factors. Independent variables were included in the logistic regression if their distribution between QoL categories differed at a probability level of p≤0.05 in univariate analyses. A probability threshold of ≤0.05 was considered to be statistically significant. All statistical tests were carried out using the statistical software package SPSS 11.0 (SPSS Inc. Chicago IL).
Results
Characteristics of the study population
The characteristics of the 414 patients are shown in Table 1. Two hundred seventy eight men and 136 women were included, 116 (25%) patients had a history of abuse or dependence on illegal drugs or sedatives at sometime in their life, 34 (8%) patients were seropositive for hepatitis C, 28 (7%) were chronic carriers of the HBs antigen, seven patients (2%) were HIV serology positive, and 286 (69%) presented at least one chronic somatic disorder according to the classification of Groll. One-hundred and sixty-seven (40%) patients presented a serious comorbid disease, i.e. a score of 1 to 5 according to the classification of Charlson and 85 (21%) presented an alcohol-related disease, in particular liver cirrhosis which was diagnosed in 33 (8%) patients. A lifetime psychiatric comorbidity was diagnosed in 325 (79%) patients; anxiety (independent or alcohol-induced) was the most frequent psychiatric comorbidity, diagnosed in 305 (74%) patients.
Characteristics of the study population (n=414).
| Variable | Number (%) |
|---|---|
| Age* | 43 ± 10 |
| Sex ratio (male/female) | 2.04 |
| European ethnicity | 368 (89) |
| Living alone | 159 (39) |
| Post-secondary education | 149 (38) |
| Unemployed | 239 (58) |
| Duration of regular alcohol consumption (years)° | 23 [1, 56] |
| Number of days of abstinence in the previous 6 months° | 20 [0, 140] |
| Alcohol intake (drinks/day)° | 16 [0, 60] |
| Duration of alcohol-dependence (years)° | 8 [0, 37] |
| Alcoholic father or mother | 146 (35) |
| Current smoker | 338 (82) |
| Abuse or dependence on illegal drugs | 69 (17) |
| Abuse or dependence on sedatives | 65 (16) |
| Serious comorbid disease+ | 167 (40) |
| Alcohol-related disease | 85 (21) |
| Major depressive episode | 92 (22) |
| Dysthymia | 22 (5) |
| Hypomania | 8 (2) |
| Mania | 15 (4) |
| Independent mood disorder | 116 (28) |
| Alcohol-induced mood disorder | 150 (36) |
| Panic disorder | 42 (10) |
| Agoraphobia | 69 (17) |
| Social phobia | 66 (16) |
| Obsessional-compulsive disorder | 9 (2) |
| Generalized anxiety disorder | 51 (12) |
| Post-traumatic stress disorder | 44 (11) |
| Independent anxiety disorder | 169 (41) |
| Alcohol-induced anxiety disorder | 136 (33) |
| At least one psychotic symptom | 18 (4) |
| At least one psychiatric disorder | 325 (79) |
Quality of life of patients on admission and at discharge
Fifty-four patients (13%) left our centre prematurely before the end of the inpatient programme thus their end of treatment SF-36 questionnaire was unavailable. Scores on each of the eight dimensions of the SF-36 for these patients on admission were not significantly different compared with those of the other patients.
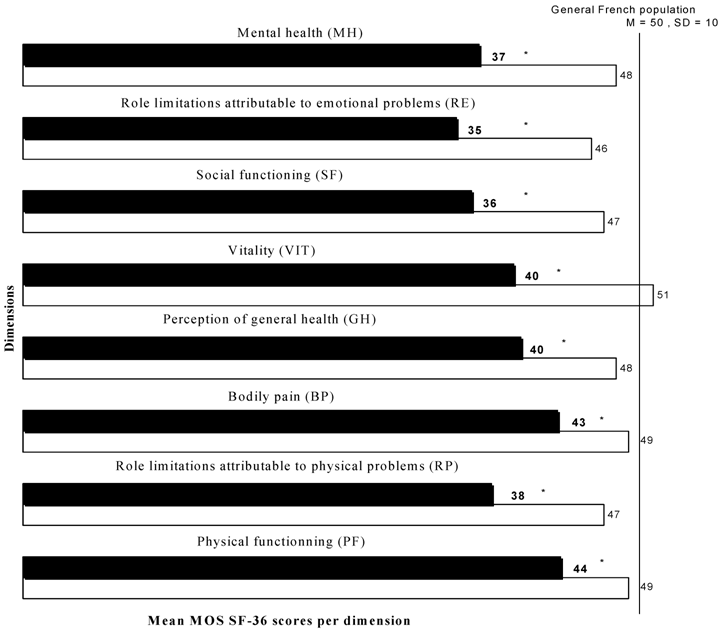
The SF-36 scores for the eight dimensions and for the Physical and Mental Component Summaries were significantly lower on admission than at discharge. On admission, the lowest scores were observed for social functioning and emotional state. At discharge, the scores for the eight dimensions were similar to those for the general French population (Figure 1).
Mean normalised scores of SF-36 dimensions for patients at admission and discharge, compared to SF-36 scores for the general French population. Filled bars: admission; open bars: discharge. *: The SF-36 scores were significantly lower on admission than at discharge (p < 0,05, Cohen's d between 0,45 and 1,1).
Predictive factors of quality of life on admission
Two-thirds of patients had a Physical Component Summary score of >42 and two-thirds of patients had a Mental Component Summary score of >25. The factors associated with a low Physical Component Summary score (≤42) on admission are shown in Table 2. The regression model including eight variables and explained 18% of the variance in score on admission (Table 2). The variables associated with a low Mental Component Summary score (≤25) on admission are shown in Table 3. The regression model including seven variables explained 20% of the total variance (Table 3).
Predictive factors of improvement in quality of life during the inpatient programme
Analysis of the distribution of the values for the differences (discharge - admission) in Physical and Mental Component Summary scores for the 360 patients followed up demonstrated an increase in Physical Component Summary of >6 points in two-thirds of patients and an increase in Mental Component Summary score of >8 points in two-thirds of patients. The variables associated with a large increase (>6) in Physical Component Summary score between admission and discharge were: a low value for this score on admission, alcohol intake ≥10 drinks/day, and the absence of somatic comorbidity (Table 4). The regression model including these five variables explained 26% of the variance. The variables associated with a large increase (>18) in Mental Component Summary score between admission and discharge were: a low value for Mental Component Summary score on admission, absence of a psychotic disorder, and the presence of abuse or dependence on illegal drugs (Table 5). The explanatory model including the six variables retained explained 19% of the variance.
Variables associated with a low Physical Component Summary score at admission (≤42). Descending step-wise logistic regression analysis, 414 patients.
| Variables tested, yes vs. no (OR=1) | Odds ratio [95%CI] | p |
|---|---|---|
| Age >45 years | 1.6 [1.1, 2.7] | 0.05 |
| Female gender | 2.1 [1.3, 3.4] | 0.002 |
| Living alone | 1.7 [1.1, 2.6] | 0.03 |
| Labourer, employee | 1.9 [1.1, 3.1] | 0.02 |
| Non-European ethnicity | 2 [0.97, 3.9] | 0.06 |
| Duration of dependence >8 years | 1.5 [0.96, 2.4] | 0.07 |
| Somatic comorbidity* | 2.5 [1.4, 4.3] | 0.001 |
| Severity of alcohol dependence >5 | 1.9 [1.2, 3] | 0.007 |
*According to the Groll's index (27)
Variables associated with a low Mental Component Summary score at admission (≤25). Descending step-wise logistic regression analysis, 414 patients.
| Variables tested, yes vs. no (OR=1) | Odds ratio [95%CI] | p |
|---|---|---|
| Severity of alcohol dependence >5 | 1.6 [1, 2.6] | 0.03 |
| Living alone | 1.1 [0.7, 1.8] | 0.6 |
| Psychiatric comorbidity | 4.5 [2, 9.5] | <0.001 |
| Abuse/dependence on sedatives | 1.2 [0.7, 2.2] | 0.6 |
| Current smoker | 2.1 [1.1, 4] | 0.03 |
| Suicidality | 2 [1.6, 4] | <0.001 |
Variables associated with a large improvement (> 6 points) in the Physical Component Summary score between admission and discharge. Descending step-wise logistic regression analysis, 360 patients.
| Variables tested, yes vs. no (OR=1) | Odds ratio [95%CI] | P |
|---|---|---|
| Severity of alcohol dependence >5 | 1.4 [0.8, 2.3] | 0.2 |
| Initial physical score ≤42 | 6.9 [4.1, 11.7] | <0.001 |
| Somatic comorbidity | 0.5 [0.3, 0.9] | 0.03 |
| Alcohol intake ≥10 drinks/day | 1.9 [1, 3.5] | 0.05 |
Variables associated with a large improvement (> 18 points) in the Mental Component Summary score between admission and discharge. Descending step-wise logistic regression analysis, 360 patients.
| Variables tested, yes vs. no (OR=1) | Odds ratio [95%CI] | P |
|---|---|---|
| Severity of alcohol dependence > 5/7 | 0.8 [0.5, 1.3] | 0.8 |
| Initial psychological summary score ≤ 25 | 4.2 [2.6, 6.9] | <0.001 |
| At least one psychotic symptom | 0.1 [0.03, 0.7] | 0.02 |
| Panic disorder | 1.1 [0.5, 2.6] | 0.8 |
| Agoraphobia | 1.8 [0.9, 3.3] | 0.06 |
| Abuse/dependence on illegal drugs | 2 [1, 3.9] | 0.05 |
Discussion
This study suggests that there is a significant improvement in all dimensions of QoL of alcohol-dependent patients after a 20-day inpatient programme for alcohol detoxification and short rehabilitation in an alcohol addiction centre. The number of DSM-IV criteria for dependence was the only factor predictive of both physical and psychological QoL scores of patients on admission.
This study shows that the QoL scores of alcohol-dependent patients on admission to hospital are much lower than those of a general reference population. Several other authors have also used the SF-36 questionnaire to measure QoL of alcohol-dependent patients and found scores to be decreased across all dimensions of the scale at the start of a treatment programme. As in our study, the scores for the psychological dimensions were reduced more than those for the physical dimensions, in particular the scores for role limitations due to emotional problems and social functioning (13, 15-19, 33, 34).
We have shown that the initial QoL of our patients was associated with several factors, stemming from the alcoholic disease itself, its consequences, and from somatic or psychiatric comorbidities. The relationship between severity of dependence and QoL of alcohol-dependent patients has been investigated by other authors by measuring the correlation between SF-36 scores and ASI (Addiction Severity Index) (9, 13, 18, 35). The pain, mental health and physical capacity dimensions appeared to be most closely correlated to ASI scores and, as in our study, the severity of dependence appeared to be the alcohol-related variable that had the strongest impact on QoL. The level of alcohol intake of patients did not appear to affect their QoL, maybe because all of our dependent patients had excessive alcohol intake. Other authors have also demonstrated that in the absence of dependence, the mode of alcohol consumption has a strong influence on QoL: heavy drinkers (at least one intake of alcohol greater than five drinks in the previous month) had a poorer QoL than other alcohol drinkers, whereas smaller regular drinkers (less than five drinks per occasion) had a better QoL than other drinkers (20, 36). We have also shown that some sociodemographic variables such as age >45 years, female gender, emotional isolation, socioprofessional category labourer or employee, had a negative relationship with QoL. Our conclusions agree with those of other authors: female gender, older age, emotional loneliness or absence of close support, low level of education, redundancy or inactivity, socioeconomic insecurity, marital or familial conflicts are the sociodemographic factors mentioned most often in the literature (10, 14, 16, 20, 37). In our study, somatic or psychiatric comorbidities to alcohol dependence significantly decreases QoL, as mentioned previously by other authors (20, 38, 39). Our study and these previous studies do not enable us to identify exactly which variables have the greatest influence on QoL. A study carried out in identical twins identified four parameters that explained the difference in QoL between alcohol-dependent twins and alcohol-dependent twins abstinent from alcohol for more than 5 years: severity of dependence, way of life (marital status, level of resources), somatic or psychological comorbidities, existence of associated dependencies (18). In our study, the presence of abuse or dependence on another substance did not affect the QoL of patients, apart from smoking for psychological QoL. Abuse or dependence on illegal drugs was associated with a large progression of Mental Component Summary Score.
The QoL of patients increased significantly during their residential stay. We have found two studies in the literature which, like ours, investigated the improvement in QoL of alcohol-dependent patients during a residential stay of 1 and 3 weeks. In both of these studies, the QoL of patients was also significantly higher at the end of their stay than on admission (40, 41). Several factors could explain this great improvement in QoL: cessation of alcohol intake, resolution of withdrawal syndrome, resocialisation of patients through various meetings and other informal exchanges during their stay, reassuring therapeutic environment, restoration of a better self-image by improvement in personal care. Other studies carried out in alcohol-dependent outpatients demonstrated an improvement in QoL when patients were abstinent (22, 23, 42-44). Apart from abstinence, our study enabled us to identify several factors linked to a favourable short-term improvement in QoL: excessive alcohol consumption and the absence of somatic comorbidity for physical QoL; abuse or dependence on illegal drugs and the absence of psychotic symptoms for psychological QoL. The improvement in QoL was more pronounced when the score on admission was low. This result demonstrates that residential care is highly effective in patients with a poor QoL on admission but also perhaps reflects rapid normalisation of QoL during therapy. In a review of the literature, we were able to find several factors that are predictive of improved QoL in alcohol-dependent patients over several weeks of residential care and in outpatients. These include regular psychosocial support, presence of a close family circle or neighbours and effective control of alcohol intake (16, 17, 43). Our results are difficult to compare with these, since our follow-up period was limited by the length of hospitalisation and was therefore much shorter. Nevertheless, they justify initiation of psychosocial support and the management of somatic or psychiatric comorbidities in patients undergoing alcohol detoxification as a strategy to improve QoL.
Several limitations exist with respect to the interpretation of the data. Firstly, our study did not permit us to differentiate between the impact of abstinence itself and that of the hospital environment on the improvement in QoL of alcohol-dependent patients. Secondly, our results do not provide an adequate demonstration of definitive improvement in QoL of alcohol-dependent patients due to the inpatient programme, since we did not follow the patients over the long-term after discharge. The short duration of follow-up (the length of hospitalisation was 19 days on average) does not allow us to predict the impact of certain variables on long- or medium-term evolution of QoL in these patients. Thirdly, the absence of a control group did not enable us to any particular aspect of care that contributed specifically to the improvement in QoL of our patients. Fourthly, thirteen percent of the patients included in our study did not complete the QoL questionnaire at the end of treatment. Their questionnaires on admission were not significantly different from those of the other patients included in the study and the proportion of these patients was similar in the three groups studied, even if this does not necessarily ensure that their QoL would have evolved the same way as those patients that remained in the programme. Finally, our results, which were obtained from a single centre, do not cover all therapeutic options and should be generalised with caution.
Conclusion
In conclusion, our study confirms the poor QoL of alcohol-dependent patients at the time of admission to hospital. Our study enabled us to identify a number of alcohol-related, sociodemographic and clinical variables linked to QoL of alcohol-dependent patients at the time of admission. We have also demonstrated the positive impact of residential care on short-term improvement in QoL of alcohol-dependent patients. These findings, if communicated to patients, could enhance their motivation to enter inpatient treatment programmes.
Conflict of Interest
The authors of this paper declare no conflict of interest.
References
1. WHO. Summary report of the working group on concepts and principles of health promotion, copenhagen 9-13 july 1984. World Health Organization Regional Office for Europe. 1984
2. Epstein RS, Sherwood LM. From outcomes research to disease management: A guide for the perplexed. Ann Intern Med. 1996;124:832-7
3. Preau M, Protopopescu C, Spire B. et al. Health related quality of life among both current and former injection drug users who are hiv-infected. Drug Alcohol Depend. 2007;86:175-82
4. Pearlman RA, Uhlmann RF. Quality of life in chronic diseases: Perceptions of elderly patients. J Gerontol. 1988;43:M25-30
5. Slevin ML, Plant H, Lynch D. et al. Who should measure quality of life, the doctor or the patient? Br J Cancer. 1988;57:109-12
6. Anderson P, Scott E. The effect of general practitioners' advice to heavy drinking men. Br J Addict. 1992;87:891-900
7. Heather N, Campion PD, Neville RG. et al. Evaluation of a controlled drinking minimal intervention for problem drinkers in general practice (the drams scheme). J R Coll Gen Pract. 1987;37:358-63
8. Zweben A, Cisler RA. Clinical and methodological utility of a composite outcome measure for alcohol treatment research. Alcohol Clin Exp Res. 2003;27:1680-5
9. Donovan D, Mattson ME, Cisler RA. et al. Quality of life as an outcome measure in alcoholism treatment research. J Stud Alcohol Suppl. 2005:119-39
10. Foster JH, Powell JE, Marshall EJ. et al. Quality of life in alcohol-dependent subjects--a review. Qual Life Res. 1999;8:255-61
11. Longabaugh R, Mattson ME, Connors GJ. et al. Quality of life as an outcome variable in alcoholism treatment research. J Stud Alcohol Suppl. 1994;12:119-29
12. Blow FC, Walton MA, Barry KL. et al. The relationship between alcohol problems and health functioning of older adults in primary care settings. J Am Geriatr Soc. 2000;48:769-74
13. Daeppen JB, Krieg MA, Burnand B. et al. Mos-sf-36 in evaluating health-related quality of life in alcohol-dependent patients. Am J Drug Alcohol Abuse. 1998;24:685-94
14. Foster JH, Peters TJ, Kind P. Quality of life, sleep, mood and alcohol consumption: A complex interaction. Addict Biol. 2002;7:55-65
15. Garg N, Yates WR, Jones R. et al. Effect of gender, treatment site and psychiatric comorbidity on quality of life outcome in substance dependence. Am J Addict. 1999;8:44-54
16. Morgan MY, Landron F, Lehert P. Improvement in quality of life after treatment for alcohol dependence with acamprosate and psychosocial support. Alcohol Clin Exp Res. 2004;28:64-77
17. Morgan TJ, Morgenstern J, Blanchard KA. et al. Health-related quality of life for adults participating in outpatient substance abuse treatment. Am J Addict. 2003;12:198-210
18. Romeis JC, Waterman B, Scherrer JF. et al. The impact of sociodemographics, comorbidity and symptom recency on health-related quality of life in alcoholics. J Stud Alcohol. 1999;60:653-62
19. Stein MD, Mulvey KP, Plough A. et al. The functioning and well being of persons who seek treatment for drug and alcohol use. J Subst Abuse. 1998;10:75-84
20. Volk RJ, Cantor SB, Steinbauer JR. et al. Alcohol use disorders, consumption patterns, and health-related quality of life of primary care patients. Alcohol Clin Exp Res. 1997;21:899-905
21. Welsh JA, Buchsbaum DG, Kaplan CB. Quality of life of alcoholics and non-alcoholics: Does excessive drinking make a difference in the urban setting? Qual Life Res. 1993;2:335-40
22. Amodeo M, Kurtz N, Cutter HS. Abstinence, reasons for not drinking, and life satisfaction. Int J Addict. 1992;27:707-16
23. Kraemer KL, Maisto SA, Conigliaro J. et al. Decreased alcohol consumption in outpatient drinkers is associated with improved quality of life and fewer alcohol-related consequences. J Gen Intern Med. 2002;17:382-6
24. Crews TM, Sher KJ. Using adapted short masts for assessing parental alcoholism: Reliability and validity. Alcohol Clin Exp Res. 1992;16:576-84
25. Sheehan DV, Lecrubier Y, Sheehan KH. et al. The mini-international neuropsychiatric interview (m.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for dsm-iv and icd-10. J Clin Psychiatry. 1998;59(Suppl 20):22-33
26. Charlson ME, Pompei P, Ales KL. et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373-83
27. Groll DL, To T, Bombardier C. et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58:595-602
28. Tarlov AR, Ware JEJr, Greenfield S. et al. The medical outcomes study. An application of methods for monitoring the results of medical care. JAMA. 1989;262:925-30
29. Sullivan EV, Pfefferbaum A. Neuroimaging of the wernicke-korsakoff syndrome. Alcohol Alcohol. 2009;44(2):155-65
30. Jenkinson C, Coulter A, Wright L. Short form 36 (sf36) health survey questionnaire: Normative data for adults of working age. BMJ. 1993;306:1437-40
31. Ware J, Kosininski M, Dewey J. How to score version 2 of the sf-36 health survey. Richemond: Quality Metric Incorporated, Lincoln. 2000
32. Leplège A, Ecosse E, Pouchot J. et al. Le questionnaire mos sf-36. Manuel de l'utilisateur et guide d'interprétation des scores. Paris, France: Editions Scientifiques Techniques et Médicales. 2001
33. Johnson JG, Spitzer RL, Williams JB. et al. Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: Findings of the prime md-1000 study. J Consult Clin Psychol. 1995;63:133-40
34. McKenna M, Chick J, Buxton M. et al. The seccat survey: I. The costs and consequences of alcoholism. Alcohol Alcohol. 1996;31:565-76
35. Butler SF, Budman SH, Goldman RJ. et al. Initial validation of a computer-administered addiction severity index: The asi-mv. Psychol Addict Behav. 2001;15:4-12
36. Okoro CA, Brewer RD, Naimi TS. et al. Binge drinking and health-related quality of life: Do popular perceptions match reality? Am J Prev Med. 2004;26:230-3
37. Beattie MC, Longabaugh R, Elliott G. et al. Effect of the social environment on alcohol involvement and subjective well-being prior to alcoholism treatment. J Stud Alcohol. 1993;54:283-96
38. Patience D, Buxton M, Chick J. et al. The seccat survey: Ii. The alcohol related problems questionnaire as a proxy for resource costs and quality of life in alcoholism treatment. Study of socio-economic consequences and costs of alcoholism and treatment. Alcohol Alcohol. 1997;32:79-84
39. Spitzer RL, Kroenke K, Linzer M. et al. Health-related quality of life in primary care patients with mental disorders. Results from the prime-md 1000 study. JAMA. 1995;274:1511-7
40. Berglund K, Berggren U, Bokstrom K. et al. Changes in mental well-being during minnesota treatment. Nord J Psychiatry. 2004;58:383-8
41. Bertholet N, Daeppen JB. A possible way to motivate ambivalent patients to undergo detoxification. Alcohol Alcohol. 2006;41:205
42. Foster JH, Peters TJ, Marshall EJ. Quality of life measures and outcome in alcohol-dependent men and women. Alcohol. 2000;22:45-52
43. Pelc I, Ansoms C, Lehert P. et al. The european neat program: An integrated approach using acamprosate and psychosocial support for the prevention of relapse in alcohol-dependent patients with a statistical modeling of therapy success prediction. Alcohol Clin Exp Res. 2002;26:1529-38
44. Watson CG, Hancock M, Gearhart LP. et al. A comparative outcome study of frequent, moderate, occasional, and nonattenders of alcoholics anonymous. J Clin Psychol. 1997;53:209-14
Author contact
![]() Correspondence to: Henri-Jean Aubin, Centre d'Enseignement, de Recherche et de Traitement des Addictions, Hôpital Paul Brousse, Assistance Publique-Hôpitaux de Paris, 94804 Villejuif, France. henri-jean.aubinap-hop-paris.fr
Correspondence to: Henri-Jean Aubin, Centre d'Enseignement, de Recherche et de Traitement des Addictions, Hôpital Paul Brousse, Assistance Publique-Hôpitaux de Paris, 94804 Villejuif, France. henri-jean.aubinap-hop-paris.fr

 Global reach, higher impact
Global reach, higher impact